Economic Implications of Increased Breastfeeding Rates in WIC
- by Victor Oliveira, Mark Prell and Xinzhe Cheng
- 2/14/2019
Highlights
- If breastfeeding rates in WIC had increased to medically recommended levels in 2016, the number of mothers who participated monthly in WIC would have increased, and program costs that year would have risen by an estimated $252.4 million.
- These higher WIC costs would have been partially offset by an estimated $111.6 million in savings on Federal Medicaid costs associated with improved health outcomes of breastfeeding women and infants.
- Estimated annual health-related cost savings accruing to WIC households, or their non-Medicaid health insurance providers, would have totaled $9.0 billion.
The U.S. Senate Committee on Appropriations in March 2018 directed ERS to conduct a study on the economic benefits of breastfeeding, including effects on WIC and Medicaid costs. WIC refers to the Special Supplemental Nutrition Program for Women, Infants, and Children administered by USDA's Food and Nutrition Service. ERS researchers found that higher levels of breastfeeding would raise WIC program costs. On the other hand, higher WIC breastfeeding rates would reduce current and future health-related costs for mothers and infants participating in WIC.
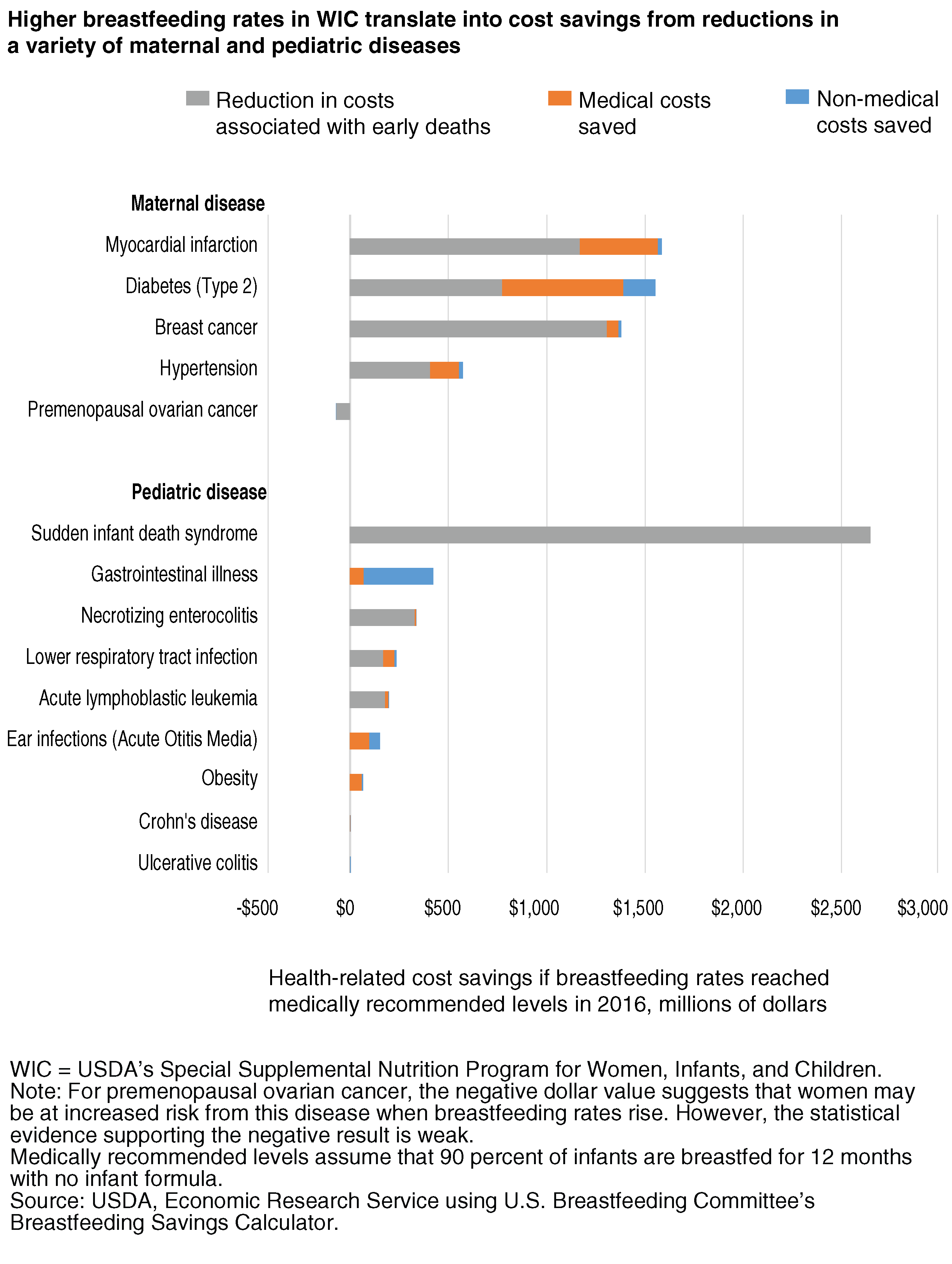
Breastfeeding offers health benefits to both infant and mother. According to the U.S. Breastfeeding Committee, infants who are breastfed have reduced risks of a number of diseases including sudden infant death syndrome (SIDS), ear and respiratory infections, and gastro-intestinal illness. Mothers who breastfeed have a reduced risk for various diseases including myocardial infarction, diabetes, and breast cancer. These health benefits can translate into economic benefits such as lower medical costs or fewer sick days away from work.
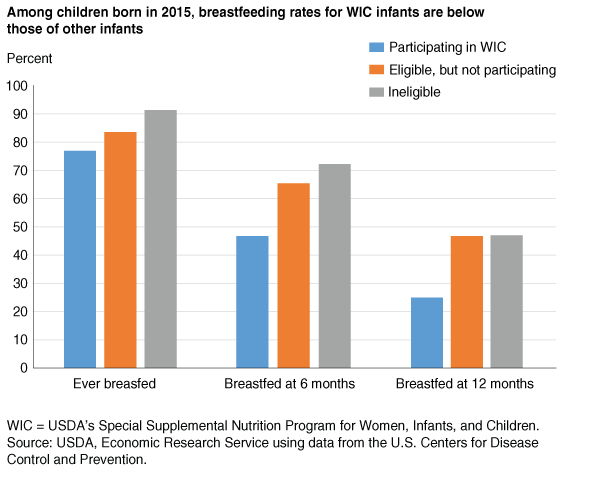
The American Academy of Pediatrics and other U.S. health organizations recommend exclusive breastfeeding for about 6 months, followed by continued breastfeeding until at least 12 months of age as complementary foods are introduced. However, breastfeeding rates in the United States—in particular for duration and exclusivity—fall short of recommended levels. Data from the U.S. Centers for Disease Control and Prevention indicate that while 83 percent of U.S. infants born in 2015 started to breastfeed, 58 percent were breastfed at 6 months and 36 percent were breastfed at 12 months. Breastfeeding rates among infants participating in WIC in 2015 were below those of low-income nonparticipating infants and infants in higher income households not eligible for WIC.
In response to the Congressional directive to study the economic benefits of breastfeeding, ERS researchers estimated the economic impacts if 90 percent of WIC infants in 2016 were breastfed for 12 months and received no infant formula during that time. The 90-percent level takes the medically recommended level of universal breastfeeding and assumes that 10 percent of mothers participating in WIC are unable to breastfeed.
Increased Breastfeeding Would Raise the Monthly Number of WIC Participants…
WIC is the Nation’s third-largest food assistance program, trailing only the Supplemental Nutrition Assistance Program (SNAP) and the National School Lunch Program. WIC provides supplemental foods, nutrition education, breastfeeding support, and referrals to health and social services to low-income, nutritionally at-risk pregnant, breastfeeding, and postpartum women; infants; and children up to age 5. WIC is based on the premise that early intervention during critical times of growth and development can help prevent future medical and developmental issues.
To be eligible for WIC, an applicant must be at nutritional risk and have an annual household income at or below 185 percent of the Federal poverty guidelines (for example, the Federal poverty guideline for a family of four in July 2018 was $25,100). A person automatically meets the income eligibility requirement if the individual participates in SNAP, Medicaid, or Temporary Assistance for Needy Families (TANF).
WIC has a wide reach. In fiscal 2016, WIC served almost 1.9 million infants per month (48 percent of all U.S. infants) and 1.1 million postpartum women per month (28 percent of all U.S. postpartum women). While breastfeeding mothers can participate in WIC for 12 months postpartum to supplement maternal diet during breastfeeding, Federal regulations limit the participation of nonbreastfeeding mothers to 6 months postpartum. In fiscal 2016, 47 percent of the 1.1 million mothers receiving WIC benefits each month were not breastfeeding and therefore did not participate in WIC after 6 months postpartum. If breastfeeding rates were to rise to medically recommended levels, the number of mothers eligible to participate in WIC for 12 months instead of 6 months would rise, increasing the average number of mothers eligible for WIC each month.
ERS researchers estimated that if WIC breastfeeding rates had increased from 2016 levels (e.g., 45 percent at 6 months of age and 25 percent at 12 months of age) to medically recommended levels (90 percent for 12 months), almost 646,000 additional mothers would have participated in WIC each month—an 8-percent increase in the total average monthly number of women, infants, and children participating in WIC. Since infants in WIC can participate for their entire first year, the number of infants participating per month is unaffected if breastfeeding rates increase.
…and Increase WIC Program Costs
Federal spending on WIC totaled $6.0 billion in fiscal 2016. Almost one third was for nutrition services and administration, including costs related to breastfeeding promotion and support, nutrition education, certification of participants, referrals to other health care and social services, and overhead and management (see box "Breastfeeding Promotion and Support Activities in WIC"). Food packages accounted for about two-thirds of total program costs.
The types and amounts of foods included in the packages for infants and mothers differ by their breastfeeding status and, for infants, by their age (measured in months), and for mothers, by months postpartum. Fully breastfeeding packages are for infants and mothers who do not receive formula through WIC. Partially breastfeeding packages are for infants and mothers who mostly breastfeed but who receive some formula through WIC. Fully formula feeding packages are for infants and mothers who do not breastfeed or only breastfeed a minimal amount. As a result, the monthly per participant food package costs vary by breastfeeding status and age/months postpartum.
For infants, the fully breastfeeding food packages are the least expensive, and the food packages for fully formula-fed infants are the most expensive for each of the 12 months (fully breastfed infants do not receive a WIC food package until they are 6 months old). For example, the estimated average monthly cost of the food package for a 6-month-old infant in 2016 was $34.66 if fully breastfed, $37.36 if partially breastfed, and $57.05 if fully-formula fed.
For mothers, the opposite is true. In recognition of the increased nutrient and calorie needs of a breastfeeding mother and to incentivize mothers to breastfeed, the fully breastfeeding packages provide additional foods such as cheese and canned fish and greater quantities of other foods such as milk and eggs. As a result, the food packages for fully breastfeeding mothers are the most expensive, and the food packages for non-breastfeeding women are the least expensive. For example, the estimated average monthly cost as redeemed of the food package for mothers at 5 months postpartum in 2016 was $48.01 for fully breastfeeding mothers, $37.14 for partially breastfeeding mothers, and $30.14 for nonbreastfeeding mothers. Further, fully breastfeeding mothers are eligible to participate up to 12 months postpartum; fully formula feeding mothers are not eligible to participate after 6 months postpartum.
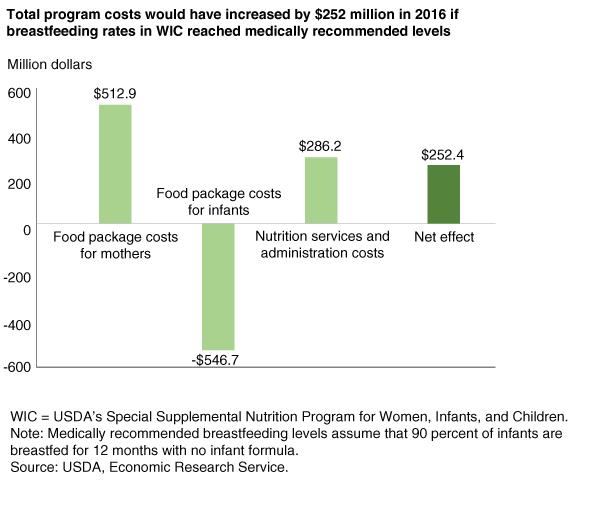
Under the scenario where breastfeeding rates in WIC increased from 2016 levels to medically recommended levels, food package costs for infants would decrease by an estimated $546.7 million. However, because of the increase in the number of participating mothers and the higher costs of the food packages for breastfeeding mothers, total food package costs for mothers would increase by an estimated $512.9 million. As a result, food package costs for mothers and infants combined would decrease by $33.8 million if medically recommended breastfeeding rates had been reached that year.
Like food packages, costs for nutrition services and administration vary by participant category. For example, in 2016, these costs averaged $19.29 per month for nonbreastfeeding postpartum women and, due in part to the cost of breastfeeding promotion and support, $29.71 for pregnant and breastfeeding women. This higher cost for breastfeeding women, along with the additional mothers participating in WIC per month, would increase nutrition services and administration costs in 2016 by $286.2 million if medically recommended breastfeeding rates had been reached that year.
The estimated net effect of increased breastfeeding rates on WIC program costs would be an increase of $252.4 million. This would represent an increase of 4 percent in total WIC costs in fiscal 2016.
Health-Related Economic Benefits Would Accrue to WIC Households from Higher Breastfeeding Rates…
The economic impacts of increased breastfeeding rates in WIC extend beyond the program’s cost. Because breastfeeding is associated with numerous health benefits, increased breastfeeding among WIC participants reduces health-related costs for WIC households and/or their health insurance providers (government or private).
The U.S. Breastfeeding Committee, an independent nonprofit organization, has developed a web-based Breastfeeding Savings Calculator, which produces estimates of the cost savings from improved breastfeeding rates for the U.S. population using evidence from the nutrition and medical literature. For nine pediatric and five maternal diseases, the calculator estimates the number of cases—and deaths if applicable—averted due to increased breastfeeding initiation, duration, and exclusivity. Then, from the number of averted diseases and deaths, the calculator computes savings from reducing three types of costs:
- Medical costs, such as physician fees and hospital costs, along with costs for prescription drugs and medical supplies. Medical expenditures are a cost whether they are paid directly by a household, an insurance company, or a government program such as Medicaid.
- Non-medical costs, mainly resulting from lost wages from missed work while a mother recovers from an illness or while a parent takes care of an ill infant or child.
- Costs of early deaths, resulting from cases of diseases that increase the risk of death. Such deaths are early in the sense that under improved health, the risk of death would be lower, adding to longevity. Monetary values can be placed, at least roughly, on these changes in the risks to life. The calculator values the cost of an early death at about $3 million to $13.5 million depending on age when the early death occurs. These values are based on people’s willingness to pay for small reductions in risk to life, which are then extrapolated to an equivalent value for the random loss of one life in a large group of people.
ERS researchers modified the calculator by incorporating data on the number of infants in WIC and the breastfeeding rates of infants and mothers in WIC, and they set the target breastfeeding rate for infants and mothers in WIC at 90 percent for 12 months.
Findings from the study indicate that if mothers in WIC households were to increase breastfeeding rates from their 2016 levels to medically recommended levels, health-related cost savings would total about $9.1 billion. Medical cost savings account for $1.5 billion of the total cost savings, while non-medical cost savings account for another $0.6 billion. Reductions in early deaths of mothers and infants account for $6.9 billion—or over three-quarters—of the total cost savings from the assumed higher breastfeeding rates among mothers participating in WIC in 2016. Because the averted early deaths of the WIC mothers occur in later years, i.e., after 2016, economic discounting was used to convert future values to 2016 values.
Reductions in the five maternal diseases combined account for $5.0 billion, or 55 percent of the total $9.1 billion health-related cost savings in 2016. Reduction in three maternal diseases—breast cancer, type 2 diabetes, and myocardial infarction—contributed $1.4 billion to $1.6 billion each in estimated benefits, with the savings from preventing early deaths exceeding the combined savings in medical and non-medical costs.
Reductions in the nine pediatric diseases combined account for $4.1 billion, or 45 percent, of total 2016 cost savings. Decreases in sudden infant death syndrome (SIDS) accounted for most of the cost savings from reduced pediatric diseases. Gastrointestinal illness, at $422 million, has the second highest cost savings. This disease was an exception in that its cost savings result primarily from a reduction in non-medical costs, reflecting that many parents take time off from work to care for infants with this common, but not medically costly, disease.
…and Federal Medicaid Costs Would Drop
Some of the estimated cost savings from increased breastfeeding would go directly to the pockets and budgets of WIC households. Parents would not lose wages from missed work, and households would have lower out-of-pocket medical costs. Some portion of the reduced medical costs would accrue to private or government health insurers, to the degree that WIC participants are covered by health insurance plans. In the case of Medicaid, taxpayers receive the savings rather than WIC households.
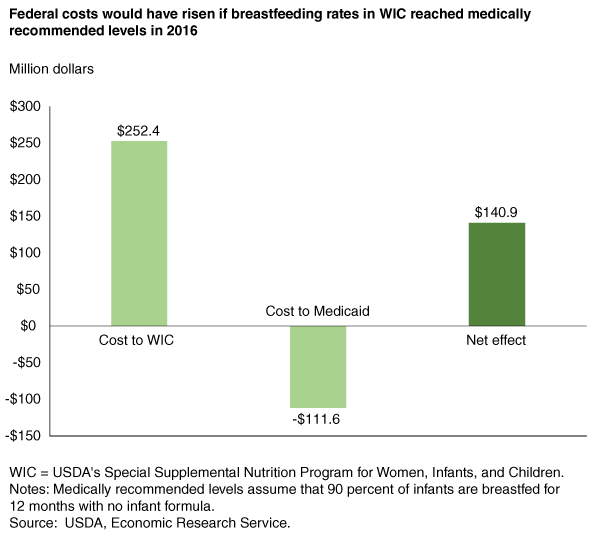
In 2016, an estimated 71 percent of WIC participants participated in Medicaid, which provides health care coverage to eligible low income individuals. To estimate cost savings to Medicaid resulting from increased breastfeeding rates among WIC participants, ERS researchers began by multiplying the total savings in medical costs attributed to higher breastfeeding rates in WIC ($1.5 billion) by the estimated share of WIC participants who participate in Medicaid (0.71).
Some of the diseases included in the study have long time horizons—in particular, maternal diseases such as breast cancer—that may not occur until many years have passed. Because some WIC participants who concurrently participate in Medicaid do not remain on Medicaid in the long-run, the study estimated the short-run savings to Medicaid due to increased breastfeeding rates in WIC that would accrue while the participant was still likely to be enrolled in Medicaid. To do so, the analysis was restricted to the five pediatric diseases with a short time horizon: ear infection, gastrointestinal illness, lower respiratory tract infection, acute lymphoblastic leukemia, and necrotizing enterocolitis. Results of the analysis indicate that if breastfeeding rates in WIC increased to medically recommended levels in 2016, estimated savings to Medicaid would total at least $176.2 million.
Medicaid is funded jointly by States and the Federal Government, with the Federal Government providing 63.3 percent of the program’s funding in 2016. As a result, the Federal share of the savings in Medicaid from higher breastfeeding rates in WIC was estimated to be $111.6 million in 2016 with the States saving $64.7 million.
Subtracting the Federal savings in Medicaid ($111.6 million) from the increased Federal program costs for WIC ($252.4 million) yields an estimated net increase in Federal expenditures of $140.9 million if mothers participating in WIC had breastfed their infants at medically recommended levels in 2016. This net increase in Federal expenditures does not include the savings from reduced non-Federal medical costs and non-medical costs ($2.0 billion) and the value of averted early deaths ($6.9 billion) from the better and extended health of mothers and infants participating in WIC.
An Alternative Scenario Based on Healthy People 2020 Targets
This study examined the economic impacts if breastfeeding rates for infants receiving WIC benefits in 2016 had hypothetically increased to levels recommended by the American Academy of Pediatrics and other U.S. health organizations (defined in this study as 90 percent of infants breastfed for 12 months). However, achieving this ambitious goal would require substantial increases in the prevalence of breastfeeding and increased investment in breastfeeding support. In 2015, 44.5 percent of infants receiving WIC benefits were breastfed at 6 months, and just 25.4 percent were still breastfed by 12 months. This large gap between current and recommended breastfeeding levels raises questions about the likelihood that medically recommended breastfeeding rates can be achieved in the near future given the current level of investment in breastfeeding promotion and support activities.
ERS researchers also examined economic impacts under several different scenarios. In each scenario, hypothesized breastfeeding rates for infants and mothers participating in WIC in 2016 increased but by less than the medically recommended levels. In one of these scenarios, WIC breastfeeding rates were assumed to reach the goals specified in the U.S. Department of Health and Human Services' Healthy People 2020, a set of national objectives for improving the health of all Americans.
Healthy People 2020 has five breastfeeding targets, including 60.6 percent at 6 months and 34.1 percent at 12 months. Under this Healthy People 2020 scenario, estimated average monthly participation in WIC would grow by 3.6 percent; WIC costs would rise by 1.6 percent, or $94.1 million; Federal Medicaid costs would fall by $15.4 million; and savings from health related costs, including medical costs, non-medical costs, and costs from early deaths would have totaled $2.4 billion. Compared to the medically recommended breastfeeding scenario, these more modest cost savings are expected given that the Healthy People 2020’s targets—which are considered to be challenging yet achievable—with regard to breastfeeding are relatively close to current breastfeeding levels.
This article is drawn from:
- Oliveira, V., Prell, M. & Cheng, X. (2019). The Economic Impacts of Breastfeeding: A Focus on USDA’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). U.S. Department of Agriculture, Economic Research Service. ERR-261.