Consumers Behaved Rationally, If Belatedly, After Food Safety Recalls in 2011 and 2012

Highlights:
-
U.S. consumers responded to a 2011 recall of cantaloupes, temporarily reducing purchases of cantaloupes and substituting honeydew and watermelon, but did not respond to a 2012 recall.
-
The two causes of contamination were different—the first was a relatively uncommon pathogen that often has fatal consequences and the second pathogen was more common, causing serious but less frequently fatal illnesses.
-
Purchases of cantaloupes and other melons shifted measurably in 2011 but not in 2012, indicating that many consumers distinguished between the two food safety risks.
When Federal health and safety officials recall a food product and warn consumers that the safety of that food has been compromised, do consumers understand that not all risks are alike? Or, do all warnings induce the same market response because consumers cannot discriminate among pathogens and the associated risk? Uncertainty about how consumers will respond to a warning or a recall is a challenge for public health officials. Aggressive communication might be called for if consumers do not understand enough of the officials’ message to recognize when risks are so large they really have to avoid a particular food. On the other hand, if consumers overestimate small or conditional risks, warnings and recalls might induce consumers to unnecessarily flee from safe foods, financially damaging parts of the food supply chain.
Although there are numerous studies of consumers’ responses to a wide range of health risks, most focus on a single risk or particular way in which food safety might have been compromised. They do not address a basic policy question: do consumers treat bigger risks as bigger problems? A recent ERS analysis used grocery store purchase data to examine whether consumers make systematic choices that take into account differences among health risks. In September 2011 and in August 2012, the U.S. Centers for Disease Control and Prevention (CDC) and the U.S. Food and Drug Administration (FDA) issued warnings to consumers to avoid particular types of cantaloupes because the fruit could cause gastrointestinal illness. The first warning related to a lesser known but often fatal illness (listeriosis) and the second related to a more common but less frequently fatal illness (salmonellosis).
These two warnings, distinct but proximate in time and identifying cantaloupe as the disease source, enable an unhappy natural experiment. The paired events make it possible to investigate whether consumers think that all gastrointestinal illness risks are alike and react in the same manner. Or, do consumers make purchase decisions that differentiate among pathogens and relative health risks?
Market Conditions Were Similar…
The warnings occurred under similar market conditions, sweeping away many factors that might complicate making comparisons. The information pointing to cantaloupes as the likely cause of a listeriosis outbreak began to be assembled in early September 2011. On September 9, the Colorado Department of Public Health and Environment advised persons in Colorado at high risk for listeriosis to avoid eating cantaloupes. On September 12, CDC advised that people throughout the mainland United States at high risk for listeriosis—including older adults, persons with weakened immune systems, and pregnant women—not eat cantaloupes from the Rocky Ford region of Colorado. The warning was quickly revised to specify Jensen Farms as the source of the contamination and that Jensen Farms had voluntarily recalled its Rocky Ford cantaloupe.
In 2010, before the recalls occurred, Colorado cantaloupe shipments accounted for less than 1 percent of U.S. annual cantaloupe shipments. Colorado farmers ship cantaloupes in July, August, and September. According to 2010 data, just 7 percent of their annual shipments occur in September; by then, almost all U.S. cantaloupe shipments are from California. At the time of the September 2011 warning, most of Colorado’s cantaloupe production was already through the supply chain.
Further, Jensen Farms’ cantaloupes were labeled as such, so the recalled product was easily distinguished from other cantaloupe. Even if consumers had followed the initial advice to avoid all Colorado cantaloupe, the Colorado share of supply at the time of the outbreak was also small. That is, the vast majority of the cantaloupe market was immediately absolved of guilt. Of course, shaken buyer confidence might still compromise sales and revenue of other cantaloupe producers.
The recall related to the Salmonella pathogen in 2012 occurred under similar market conditions—a discrete farm providing a small share of total U.S. cantaloupes. The recall identified Chamberlin Farms Produce, Inc., of Owensville, Indiana, as the source of the multistate outbreak. Indiana shipments accounted for 1.4 percent of U.S. 2010 cantaloupe shipments. Indiana farmers ship cantaloupes in July (91 percent of Indiana shipments in 2010) and August (9 percent). The event began in August 2012. Again, most of Indiana’s cantaloupe production had shipped before any information about the outbreak surfaced. Also, like the 2011 recall, a single farm was identified as the source of contamination, greatly simplifying removal of the recalled product from commerce.
… Risks Were Not
While the market conditions under which the two recalls occurred were remarkably similar, the risk posed by exposure to Salmonella usually is less dire than the risk posed by exposure to Listeria. Most people infected with Salmonella develop diarrhea, fever, and abdominal cramps 12 to 72 hours after infection. The illness usually lasts 4 to 7 days, and most persons recover without treatment. However, in some cases the diarrhea may be so severe that the patient needs to be hospitalized. In a limited number of these patients, the Salmonella infection may spread from the intestines to the blood stream, which can cause death. The elderly, infants, and those with impaired immune systems are more vulnerable to this outcome.
CDC describes Salmonella as causing 1 million illnesses in the United States each year, along with 19,000 hospitalizations and 380 deaths. Less than 2 percent of those who fall ill require hospitalization. Many milder cases are not diagnosed or reported. So, many Americans likely had direct experience with the symptoms of salmonellosis before 2012, and most returned to robust good health.
The risk posed by Listeria is more life threatening. Almost everyone diagnosed with listeriosis has an invasive infection in which the bacteria spread beyond the gastrointestinal tract. In older adults and people with compromised immune systems, listeriosis can develop into septicemia and meningitis. A pregnant woman sickened with listeriosis can have a miscarriage or a baby born with bacteremia and meningitis. CDC estimates that approximately 1,600 illnesses and 260 deaths due to listeriosis occur annually in the United States.
CDC’s tally of the 2012 Salmonella outbreak from cantaloupe included 261 illnesses, 3 deaths, and 94 hospitalizations. The Listeria event 1 year earlier caused 147 illnesses, 33 deaths, and a 99-percent hospitalization rate among those who fell ill. One miscarriage was reported. The 2011 Listeria outbreak mostly afflicted the elderly, with 78 the median age of those who fell ill.
Consumers Received Information Through Familiar Sources But Sought More
The 2011 listeriosis outbreak surprised U.S. health professionals. Listeria had emerged as a problem in the 1980s with processed meat, with outbreaks from hot dogs and deli meats during the 1990s. The 2011 outbreak was the first listeriosis outbreak associated with melon: the pathogen had found a new way into the food supply.
The news media responded to the new public health problem by devoting more news stories and coverage time to the listeriosis outbreak than to the salmonellosis outbreak. News stories reported that the listeriosis pathogen had an especially high fatality rate and was especially hazardous for the elderly and pregnant women. A search of the Vanderbilt Television News Archive (VTNA) yielded 11 evening news broadcasts on the listeriosis outbreak beginning on September 14, 2011, and ending on October 19, 2011. The VTNA is a searchable database of news abstracts and broadcast descriptions covering ABC, CBS, NBC, CNN, and Fox News. Six broadcasts came from ABC, three from NBC, and one each from CBS and CNN for a total coverage time of 19.5 minutes.
In contrast, there were just three evening news broadcasts about the salmonellosis outbreak, with a total coverage time of 2 minutes. Four networks covered the listeriosis outbreak, versus two for the salmonellosis outbreak. Broadcasts on the listeriosis outbreak spanned 35 days, while the salmonellosis outbreak was covered for 2 days.
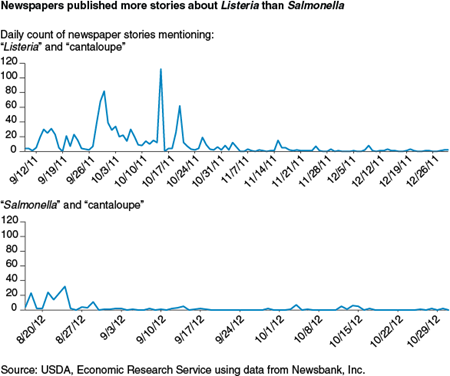
Clearly, consumers do not get all their news and information from television broadcasts. A search for articles on the listeriosis and salmonellosis outbreaks in a database of 2,273 U.S. newspapers revealed that while the listeriosis outbreak was reported immediately after the FDA warnings and recall, it was several weeks before newspaper coverage peaked: 88 news stories during the first week (September 9-September 14), 110 the following week, 138 the week after, and 240 during the week of September 30-October 5. Weekly totals dropped into double digits by the end of October but did not consistently drop to single digits until the end of December. The listeriosis outbreak continued to be reported over at least 28 weeks.
In comparison, the salmonellosis outbreak received much less attention for a much shorter time from newspapers. The first 7 days of Salmonella news coverage totaled 92 articles. The second week (August 24-August 30, 2012) totaled 50 news stories. But most successive weeks totaled in single digits.
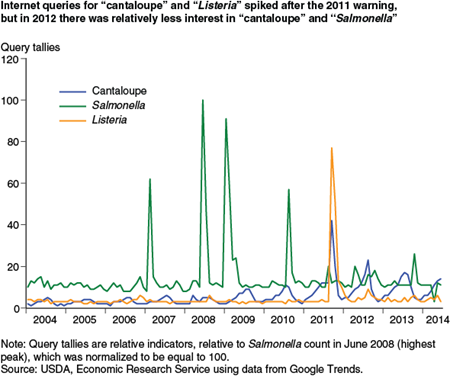
For consumers interested in relative risks, it makes sense that media would supply more information about the larger risks—those more likely to be fatal. It also makes sense that consumers would search for more information about larger risks. An analysis of Internet searches revealed that there was relatively little interest in Listeria or in cantaloupe until the September 2011 warning, after which interest in both spiked. Internet searches revealed relatively little interest in Salmonella and cantaloupe in 2012.
Google Trends, of Google Inc., is an online search tool that allows users to see how often specific keywords or phrases have been queried over a specific period of time. Internet searches for “cantaloupe” show an annual cycle of interest, peaking in summer when cantaloupe purchases are highest. Cantaloupe queries spiked in September 2011 along with Listeria, which was not much queried during the reporting period except for September 2011 and several months following.
The Salmonella series displays four large spikes, coincident with FDA’s February 2007 warnings about peanut butter products, FDA’s June 2008 warning to avoid tomatoes and other raw vegetables, regulatory actions taken in January and February 2009 regarding peanut butter, and FDA’s August 2010 egg recall. Internet searches for Salmonella around the time of the 2012 cantaloupe and salmonellosis warning were much fewer. Clearly, newspapers had many more risky issues to report, and consumers had more substantive risks to negotiate. Salmonella contaminating a small portion of the cantaloupe supply might have rationally been ignored by consumers and the news media.
Listeriosis Shifted Melon Demand, Salmonellosis Did Not
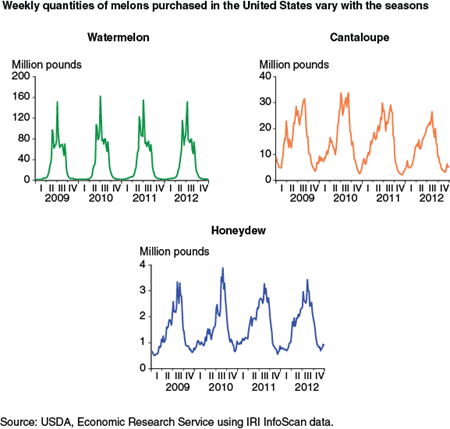
While melons can be bought year round, quantities peak in the summer months. Melon prices are lowest in the middle of the third quarter (summer) each year, when supply is greatest, and peak in early December. Peak watermelon purchases (approximately 160 million pounds per week) are 100 times higher than the lowest weekly purchases in winter (1.6 million pounds per week), whereas cantaloupe purchases range up to 35 million pounds per week in the summer and typically fall to 5 million pounds per week in the winter.
Both recalls occurred near annual peaks in quantities purchased. Even without the warnings, quantities purchased were likely to fall in the succeeding weeks. That is, comparing quantities purchased in the weeks before and after the warnings confounds the effects of the warning with seasonal production patterns. To avoid this, demand for U.S. melons was estimated to account for these ordinary, seasonal changes in quantities purchased. Remaining changes can then be attributed to the health warnings.
ERS researchers consolidated retail sales data for 30 varieties of melons into 5 melon varieties: cantaloupe, watermelon, mini seedless watermelon (including Mickey Lee/Sugarbaby), honeydew, and all others. (“All other” melons are almost entirely specialty varieties that are purchased in small quantities at prices substantially higher than the better known varieties.) Looking across seasons, watermelon captures the largest share of the melon market whether measured in expenditures, pounds, or budget share. Across 2009 and 2010, watermelon accounted for 48.5 percent of total retail sales of melons and cantaloupe’s share was 33.1 percent. An average of 30.7 million pounds of watermelon were sold each week, and weekly cantaloupe sales were 15.2 million pounds.
In the weeks following the initial August 17, 2012, Salmonella warning, the demand model explained most of the variation in quantities purchased—trying to account for the warning added nothing. Sales of cantaloupe fell in step with prices increasing. There is nothing to indicate that consumers’ purchase patterns changed beyond the usual price sensitivity.
Consumer response to the Listeria warning is another story. Cantaloupe purchases were abnormally low for 4 weeks beginning October 9, 2011. The first major spike in newspaper articles about the Listeria warning occurred a few days before the model shows cantaloupe purchases abnormally low. U.S. cantaloupe purchases, given the prevailing market prices, were 6.2 million pounds below normal for the 4-week period. In contrast, honeydew and watermelon purchases were abnormally high for 3 weeks beginning October 2, 2011. Honeydew sales were up by a total of 1.0 million pounds (21 percent), and watermelon purchases were up 3.7 million pounds (12 percent).
Expenditures on melon varieties were also reallocated after the listeriosis outbreak. Cantaloupe purchases fell $3.9 million over the 4-week period. Honeydew and watermelon purchases increased $0.9 million and $3.2 million, respectively. Weekly expenditures on cantaloupe during October 2009 and 2010 averaged $14.4 million. The $3.9 million decline in sales in 2011 represents a 6.7-percent reduction in October sales from the previous 2 years.
When It Comes to Information, Timing Is Everything
If consumers shift their purchases in response to the magnitude of foodborne disease risks, those shifts can create financial incentives for suppliers to produce food that is safe. The problem with relying on consumers to police suppliers is that consumers usually have insufficient information about the source of contamination (or are unable or unwilling to take time to precisely identify the source of contamination). If information given to consumers precisely identifies products that are unsafe and consumers use the information to correctly discriminate between foods identified as potentially contaminated and all other foods (safe foods), consumers’ individual choices might do exactly what recalls are supposed to do—remove contaminated products from commerce. However, if consumers are not fully informed about the products identified as potentially contaminated and those that are safe, their choices might impose costs on suppliers who are blameless.
The pattern of responses to the 2011 and 2012 cantaloupe recalls suggests that consumers understood the message from Federal health and safety officials and reduced purchases of cantaloupe when they thought the risk of eating cantaloupes might be fatal. At the same time, consumers apparently parsed the warning closely and recognized that other melons were safe to consume.
In the 2011 cantaloupe recall over Listeria, however, the demand shifts were too late to accomplish the goals of the recall. Demand shifts between types of melons occurred a month after the recall and the warning. By that time, almost all the illnesses attributed to the outbreak had already occurred, and supplies were sourced outside Colorado. In sum, the costs imposed by consumers’ choices were borne by suppliers who had nothing to do with compromised food safety; shifting demand did not do much to protect consumers.
While the directions of shifts in melon demand were not unexpected, the misalignment between the recall’s timing and consumers’ response was unusual. Consumers have responded more quickly to other food safety warnings. Even so, this case points to the potential benefits from improved communication between public health officials and consumers. Consumers armed with accurate and timely information might make more suitable choices over foodborne risks. More nimble and targeted demand shifts could compel suppliers whose products are unsafe to invest more in food safety. Along with producing more safety, a side benefit would be that more knowledge about preventing foodborne illness would be produced.
For many products—especially fresh produce—these benefits are not always realized because the supply chain is so efficient that products are moved from farm to fork faster than a foodborne disease outbreak and its source can be identified. Warnings might be issued when the risk has passed and retail shelves display uncontaminated produce from suppliers who are blameless. Attaining the benefits from consumer demand shifts will require information that motivates consumers to make different food choices when risks make it appropriate to do so and will require information that is timelier—not easy or inexpensive given current foodborne illness surveillance science and the size of the U.S. food system.
How Much Does It Matter How Sick You Get? Consumers' Responses to Foodborne Disease Outbreaks of Different Severities, by Fred Kuchler, USDA, Economic Research Service, August 2015