ERS Charts of Note
Subscribe to get highlights from our current and past research, Monday through Friday, or see our privacy policy.
Get the latest charts via email, or on our mobile app for  and
and 
Tuesday, November 28, 2023
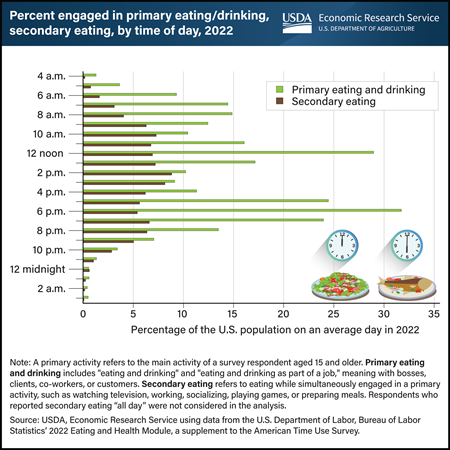
Throughout an average day in 2022, individuals aged 15 and older exhibit two distinct peak time blocks for primary eating and drinking—between 12 noon and 12:59 p.m. and from 6 to 6:59 p.m. About 3 in 10 individuals engaged in primary eating and drinking during each of these periods. While some people prefer to eat and drink while not doing anything else (primary eating and drinking), others opt for grazing while multitasking (secondary eating). Notably, between 9 a.m. and 9:59 p.m., at least 5 percent of U.S. residents participated in secondary eating each hour in 2022. The top five concurrent activities during secondary eating included watching television and movies, paid work, socializing with others, playing games, and food and drink preparation. Examining the eating patterns of the U.S. population is key to better understanding the determinants of dietary intake and diet-related health status. This data and chart come from the USDA, Economic Research Service’s Eating and Health Module (ATUS) data product, which is part of the nationally representative American Time Use Survey.
Wednesday, November 8, 2023
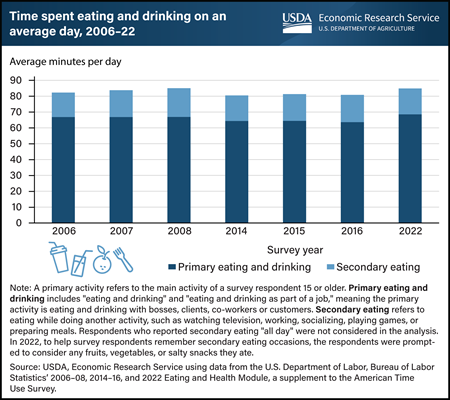
On an average day in 2022, individuals 15 and older spent 68.5 minutes engaged in eating and drinking as a “primary,” or main, activity. USDA, Economic Research Service (ERS) sponsors and maintains data on time spent eating and drinking for the Eating and Health Module, a supplement to the U.S. Department of Labor, Bureau of Labor Statistics’ American Time Use Survey (ATUS). Information about the time and location U.S. residents spend eating and drinking can offer valuable insights into how nutrition and health outcomes vary over time and can inform the design of food assistance and nutrition policies and programs. ERS researchers found that respondents devoted an extra 16.4 minutes to eating as a secondary activity, which means eating while doing something else, such as watching television, working, socializing, playing games, or preparing meals. In 2022, the top two places for primary eating and drinking and secondary eating were “own home or yard” and “workplace.” Overall, individuals in the United States aged 15 and older allocated 85 minutes to both primary eating and drinking and secondary eating on an average day in 2022. This is a modest increase of about 4 minutes compared with the survey data from 2016. This data and chart come from the ERS Eating and Health Module (ATUS) data product, which is part of the nationally representative ATUS.
Thursday, July 20, 2023
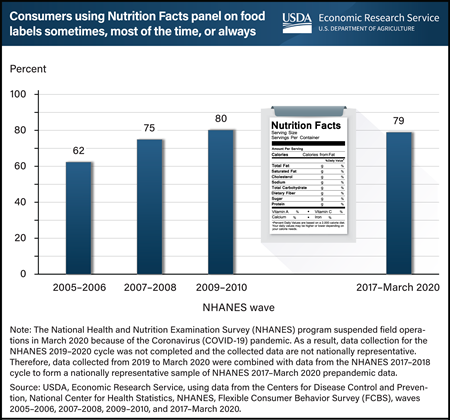
Nearly 4 out of 5 adults aged 20 and older reported they regularly used the Nutrition Facts panel when deciding to buy a food product during the most recent wave of the Flexible Consumer Behavior Survey (FCBS), from 2017 to March 2020. That is 79 percent, which is much higher than the 62 percent of adults who reported regular use of the Nutrition Facts panel in 2005–06. Regular use includes using the panel “sometimes,” “most of the time,” or “always” in food purchasing decisions. The Nutrition Facts panel on packaged foods lists the amount of calories, fat, fiber, carbohydrates, and some other nutritional information—all of which helps consumers compare products and make healthier food choices. Standardized nutrition information became accessible to U.S. consumers on almost all packaged foods sold in grocery stores, supermarkets, superstores, and other retail stores following the Nutrition Labeling and Education Act of 1990. Since 2007, USDA, Economic Research Service (ERS) has sponsored the FCBS by providing partial funding for data collection and survey administration. FCBS is a module of the National Health and Nutrition Examination Survey (NHANES), which collects information on U.S. consumers’ knowledge, attitudes, and beliefs about nutrition and food choices. This chart appears on ERS’ Flexible Consumer Behavior Survey topic page, updated in June 2023.
-FAH-Spending-by-Race_450px.png?v=9754.8)
Monday, July 10, 2023
U.S. households shifted away from buying foods at restaurants and other food service venues to food-at-home (FAH) outlets such as grocery stores and other retail establishments in 2020. The largest FAH shifts came from a category designated by USDA, Economic Research Service (ERS) as “all other FAH,” which includes prepared meals and salads, desserts, and foods not elsewhere classified such as soups, savory snacks, candy, sweeteners, margarine, and butter. “All other FAH” was by far the largest FAH category before 2020, and its share of the household food budget increased by 2.6 percentage points in 2020 compared with the period from 2016 to 2019. However, this increase was unevenly distributed across racial and ethnic populations and among subcategories within “all other FAH.” All U.S. racial and ethnic subpopulations except Hispanic households increased their total food budget share for “all other FAH” during this period. Black households increased their budget shares for “all other FAH” the most, followed by Asian households. The increase by Asian households on “all other FAH” was driven by a 1.6-percentage-point rise in prepared meals and salads and a 1.8-percentage-point increase in other, not elsewhere classified foods, such as snacks. In contrast, Black households had a larger increase in other, not elsewhere classified foods (2.0 percentage points) and desserts (1.4 percentage points). This chart appears in the ERS Amber Waves article, New Analysis Approach Illuminates Differences in Food Spending Across U.S. Populations, published in May 2023.
Tuesday, May 23, 2023
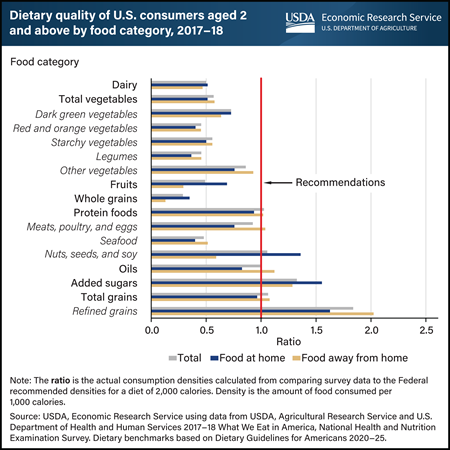
U.S. consumers’ eating patterns differ from Federal recommendations for many food categories, and where food is obtained plays a role. Researchers from USDA, Economic Research Service (ERS) and the University of Georgia examined diet patterns based on density—amounts of food consumed per 1,000 calories—using the latest available national food consumption survey data collected in 2017–18. They compared average consumption densities of 17 food categories with what would be needed to match the Dietary Guidelines for Americans recommendations, assuming a 2,000-calorie intake. Average total consumption densities for 11 food categories fell more than 20 percent outside of recommended levels, with whole grains more than 70 percent below the recommended amount. Refined grains, on the other hand, had a consumption density of more than 85 percent above the recommended level. Densities of 6 food categories were within 20 percent of the recommended range. Generally, food purchased at grocery stores, supermarkets, and similar retailers for home preparation had consumption densities more in line with dietary recommendations than food obtained from commercial away-from-home sources (primarily restaurants and fast food establishments). This chart is drawn from the ERS report Dietary Quality by Food Source and Demographics in the United States, 1977–2018, published March 2023.
Tuesday, May 2, 2023
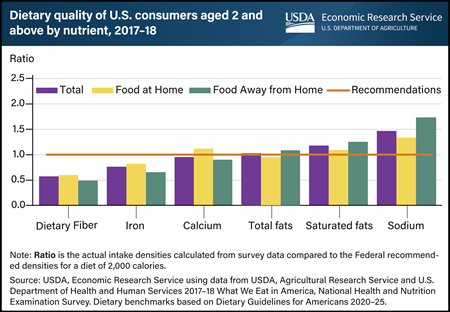
U.S. consumers’ intakes of several key nutrients differ from Federal recommendations. Differences are associated with where they obtain food. Researchers from USDA, Economic Research Service (ERS) and the University of Georgia examined diet patterns based on density—amounts of nutrients consumed per 1,000 calories—using the latest available national food consumption survey data collected in 2017–18. They compared average consumption densities of six nutrients with what would be needed to match Dietary Guidelines for Americans recommendations, assuming a typical 2,000-calorie intake. On average, intake densities of dietary fiber and iron were more than 20 percent below the recommended level; calcium densities were closer to the recommended level but still fell short of recommendations. Total fat intake was within 20 percent of the highest recommended percent of calories from total fats, which is 35 percent. The density of saturated fats for food away from home (FAFH) and densities of sodium from all sources (total, food at home, and FAFH) were more than 20 percent above the recommended limit. Generally, the nutrient densities of food purchased at grocery stores, supermarkets, and similar retailers for home food preparation were more in line with dietary guidelines recommendations than those of food obtained from commercial FAFH preparation sources (primarily restaurants and fast food establishments). This chart appears in the ERS report Dietary Quality by Food Source and Demographics in the United States, 1977–2018, published March 2023.
Tuesday, March 28, 2023
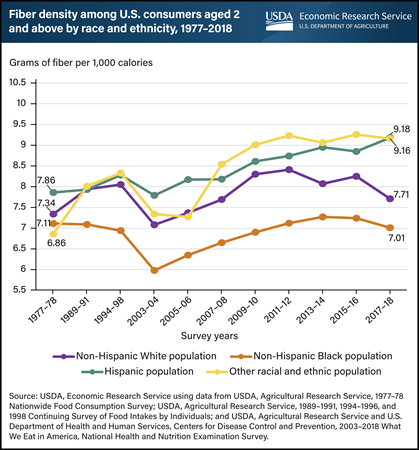
According to the 2020-2025 Dietary Guidelines for Americans, low intakes of dietary fiber are a public health concern for the general U.S. population. Improving consumption of dietary fiber may reduce risk of cardiovascular disease, type 2 diabetes, and some types of cancer. The diet of U.S. consumers averaged 8.1 grams of fiber for each 1,000 calories in 2017–18, or 58 percent of the recommended 14 grams per 1,000 calories. Researchers from USDA, Economic Research Service (ERS) and an external collaborator analyzed Federal food consumption survey data spanning the years 1977 through 2018 (the most recent available national data). They found that dietary fiber density, measured as grams of fiber per 1,000 calories in food consumed, did not vary much across race and ethnicity in the 1977–1978 and 1989–1991 survey periods, but the gap in fiber density across race and ethnicity has widened over time. Since 1994–98, the diets of non-Hispanic Black people have been significantly lower in fiber density than those of non-Black people. In 2017–18, Hispanic populations and individuals of other races and ethnicities had a diet of 9.2 grams of fiber per 1,000 calories—significantly higher than the 7.7 and 7 grams consumed by non-Hispanic White people and Black people, respectively. This chart appears in ERS’ report Dietary Quality by Food Source and Demographics in the United States, 1977–2018, published March 2023.
-Fruit-Consumption-at-School_450px.png?v=9754.8)
Wednesday, March 8, 2023
In 2017–18, meals, snacks, and other foods obtained at school were the richest source of fruit for children ages 2 to 19. These foods provided an average of 1.36 cups of fruit per 1,000 calories consumed each day. The USDA, Economic Research Service (ERS) calculated average daily consumption of food groups and selected nutrients by food sources using food consumption data collected by the USDA and Department of Health and Human Services in 2017–18, the latest year for which data are available. Food sources include foods obtained from grocery stores and similar retailers, primarily for home preparation, and foods obtained from away-from-home establishments, such as full-service and fast-food restaurants, and schools. The fruit food group includes whole fruits (fresh, canned, frozen, and dried) and 100 percent fruit juice. The Dietary Guidelines for Americans, 2020–25 recommend individuals 2 years and older consume between 1 and 2.5 cups of fruit per day, depending on age and calorie level of dietary pattern. Breakfasts and lunches from USDA’s school meal programs are required to regularly include fruit. This chart is drawn from the supplemental tables on U.S. food density published in March 2023 with the USDA, Economic Research Service report Dietary Quality by Food Source and Demographics in the United States, 1977–2018.
Monday, October 24, 2022
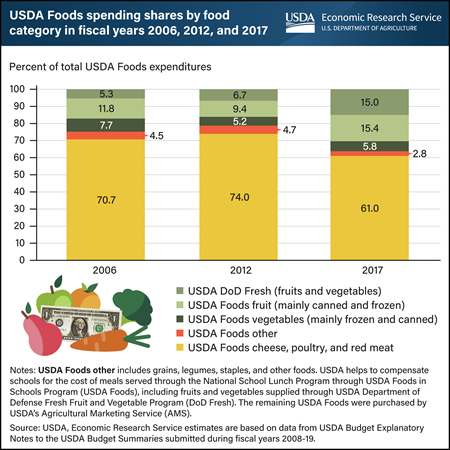
About 100,000 U.S. public and private nonprofit schools participate in the National School Lunch Program (NSLP), which served about 4.9 billion lunches in fiscal year 2019. The majority of foods served through the NSLP are bought through typical market channels, such as foodservice distributors, with USDA cash reimbursements to schools supporting their purchase. However, schools also make use of the USDA Foods in Schools Program (USDA Foods). Schools have two options for acquiring fruits and vegetables through USDA Foods: USDA Foods purchased by USDA’s Agricultural Marketing Service (AMS), which supplies mainly canned and frozen fruits and vegetables, and fresh fruits and vegetables distributed through the USDA Department of Defense Fresh Fruit and Vegetable Program (DoD Fresh). After school meal nutrition standards were updated in 2012, schools were required to serve more fruits and a wider mix of vegetables, including dark green and red/orange vegetables. Following the change in standards, schools obtained more fruits and vegetables through USDA Foods and especially through DoD Fresh. While there was no clear change in the types of foods chosen from 2006 to 2012, the percent of USDA Foods entitlement funds used for purchasing fruits and vegetables from DoD Fresh rose sharply from 6.7 percent of total USDA Foods in 2012 to 15 percent in 2017. Fruit obtained through AMS—mainly canned and frozen—rose from 9.4 percent of total USDA Foods spending in 2012 to 15.4 percent in 2017. Vegetables obtained from USDA’s AMS slightly rose from 2012 to 2017. As the percentage of spending on fruits and vegetables increased, the percentage spent on meat, poultry, and cheese dropped from nearly 74 percent in 2012 to 61 percent in 2017. This chart appears in the ERS report, Trends in USDA Foods Ordered for Child Nutrition Programs Before and After Updated Nutrition Standards, released September 1, 2022.
_450px.png?v=9754.8)
Monday, August 22, 2022
U.S. adults ages 20 and older reported a 3 percent higher prevalence of obesity during the first year of the Coronavirus (COVID-19) pandemic, according to a recent study conducted by a researcher at the USDA, Economic Research Service (ERS). The study analyzed data from the Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System from March 13, 2020, to March 18, 2021, compared to a pre-pandemic baseline period of January 1, 2019, to March 12, 2020. Four behaviors that can influence the risk of obesity—exercise, hours of sleep, alcohol use, and cigarette smoking—were also examined to help explain the change in the adult obesity rate during the pandemic. Participation in exercise rose 4.4 percent over the period and people slept 1.5 percent longer, both associated with reducing obesity. Meanwhile, the number of days in the period of a month in which alcohol was consumed was 2.7 percent higher, and cigarette smoking dropped by 4 percent. Research shows that higher alcohol intake and reduced cigarette smoking can lead to obesity and therefore may have contributed to the higher rate of obesity among U.S. adults during the pandemic. This chart appears in the ERS’s Amber Waves article, "Adult Obesity Prevalence Increased During the First Year of the COVID-19 Pandemic", published July 2022.
Tuesday, June 7, 2022
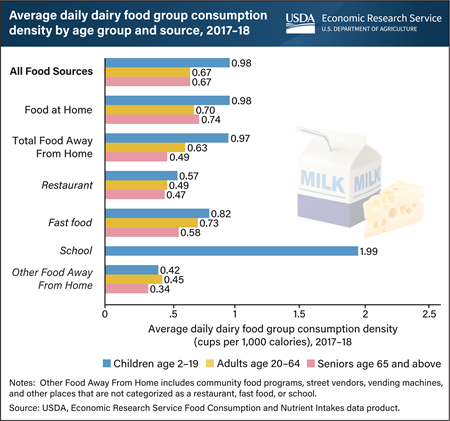
From 2017 to 2018, meals, snacks and other foods at school were the richest source of dairy for children ages 2 to 19. These foods provided an average of 1.99 cups of dairy products per 1,000 calories consumed each day. The USDA, Economic Research Service’s (ERS) Food Consumption and Nutrient Intakes data product provides calculations of the average daily consumption of food groups and selected nutrients by food sources. It uses food consumption data collected from a nationally representative sample of U.S. consumers by the USDA and the Department of Health and Human Services. Food sources are comprised of foods prepared at home and foods prepared away from home, including foods from restaurants, fast food establishments, and schools. The dairy foods group, as defined by USDA dietary guidance, is a major source of calcium and includes milk, cheese, yogurt, lactose-free milk, and fortified soy milk. The Dietary Guidelines for Americans, 2020–25, recommend individuals 2 years and older should consume 2–3 cups of dairy per day, depending on age and calorie level of dietary pattern. Although no age group meets this recommendation, children come the closest, with school foods making an important contribution. This chart was drawn from the ERS’s Amber Waves article, “Food Consumption and Nutrient Intakes Data Product Shines a Light on U.S. Diets”, September 2021.
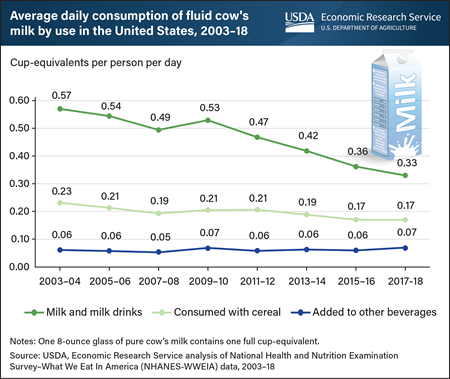
Monday, January 31, 2022
U.S. per capita consumption of fluid cow’s milk has been trending downward since about the mid-1940s, and it fell at a faster rate during the 2010s than in each of the previous six decades. Using dietary intake surveys collected between 2003 and 2018, USDA, Economic Research Service (ERS) researchers examined recent trends in milk consumption by looking at how individuals consumed the milk and consumers’ ages. Results confirmed that drinking milk as a beverage is the primary way that individuals of all ages consume fluid cow’s milk. These beverages include plain and flavored fluid milk as well as malted milk, eggnog, kefir, hot chocolate, and other milk-based beverages. On a given day in 2003–04, U.S. consumers drank about 0.57 cup-equivalents of fluid cow’s milk on average. Per person consumption of milk as a beverage fluctuated over the 2000s between 0.53 and 0.57 cup-equivalents per day. However, it declined over the 2010s, falling to 0.33 cup-equivalents in 2017–18. Over the study period, U.S. per person consumption of milk with cereal also fell by 0.06 cup-equivalents, with the steepest drop in consumption occurring among children. No significant changes were detected in the amount of milk that U.S. consumers pour into other, non-dairy beverages such as tea and coffee. This chart appears in the ERS report Examining the Decline in U.S. Per Capita Consumption of Fluid Cow’s Milk, 2003–18, released October 2021.
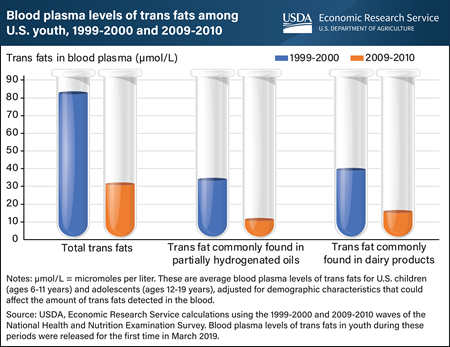
Monday, July 19, 2021
A 2020 USDA, Economic Research Service (ERS) study analyzed data publicly released for the first time in March 2019 and found that blood plasma levels of trans fats among youth fell by more than three-fifths (61.9 percent) from 1999-2000 to 2009-2010. Trans fats raise artery-clogging “bad” cholesterol (low-density lipoprotein, or LDL) levels and lower “good” cholesterol (high-density lipoprotein, or HDL) levels. Thus, increased intake of trans fats can result in an elevated risk of cardiovascular disease. The decrease in blood plasma levels of trans fats among youth came after a recommendation in the 2005 Dietary Guidelines for Americans to limit consumption of trans fats and a Federal Government requirement that trans fats content be included on packaged food labels. While young people are at a lower risk of developing cardiovascular disease than adults, intake of trans fats in early childhood and adolescence could set in motion processes that lead to the disease in adulthood. Data on blood plasma levels of trans fats of children (ages 6-11 years) and adolescents (ages 12-19 years) living in the United States were drawn from the 1999-2000 and 2009-2010 waves of the National Health and Nutrition Examination Survey, a nationally representative survey that assesses the health and nutritional status of the U.S. population. Blood plasma levels of the type of trans fat often found in partially hydrogenated oils fell by about two-thirds (67.2 percent) from 1999-2000 to 2009-2010, compared with a 60.5 percent decline in blood plasma levels of the type often found in dairy products. This chart appears in the ERS’ Amber Waves article, Trans Fat Levels Among U.S. Youth Fell From 1999 to 2010, June 2021. See also an Amber Waves finding from June 2017, Blood Levels of Trans Fats Among American Adults Fell from 1999 to 2010.
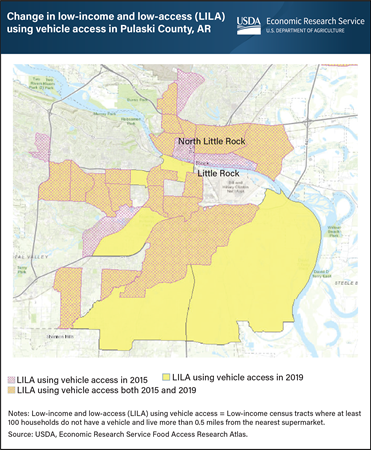
Wednesday, April 28, 2021
The USDA, Economic Research Service’s (ERS) Food Access Research Atlas provides a map of neighborhoods with limited access to nutritious, affordable food for the entire United States. Limited access to high-quality, low-cost food may impede some consumers from achieving a healthy diet. The updated Atlas allows users to map low-income and low-supermarket access census tracts for 2019 and compare the results with those for 2015. Individuals can choose to display one or several of the measures of low-supermarket access that are based on residents’ distances from the nearest supermarket (more than 0.5 or 1 mile in urban areas or more than 10 or 20 miles in rural areas) and whether a substantial number of households have access to a vehicle. One measure considers a tract to be low-income and low-access (LILA) if it is low-income and contains a substantial number of vehicle-less households that live more than 0.5 miles from the nearest supermarket. Using this measure, the number of low-income and low-access census tracts in Pulaski County, Arkansas, for example, rose 4 percent from 2015 to 2019. Twenty-three percent of Pulaski County households lived in these tracts in 2019, including 6 percent who lived more than 0.5 miles from a supermarket and did not have a vehicle. This map was created using ERS’s Food Access Research Atlas, updated April 27, 2021.
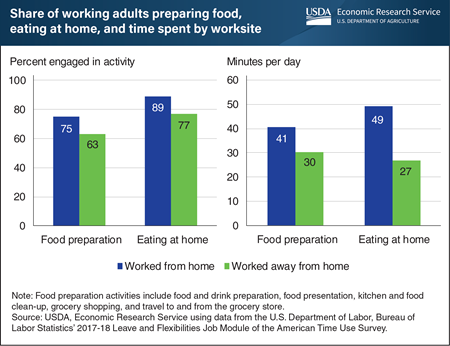
Wednesday, March 3, 2021
The U.S. Federal Government announced social distancing guidelines in March 2020 to slow the spread of COVID-19, and many U.S. jurisdictions followed by issuing stay-at-home orders. As a result, many people have been working from home since then, which prompts the question: Do individuals who work from home spend time on their daily tasks differently than those who work away from home? While USDA, Economic Research Service (ERS) researchers do not have time-use data from the COVID-19 period for the United States, analyses of past time-use patterns provide some insights. ERS researchers used data from the 2017-18 Leave and Flexibilities Job Module of the Bureau of Labor Statistics’ American Time Use Survey to study the amount of time respondents spent in food preparation and eating at home, according to the location from which they worked the day covered by the interview. They found that over an average weekday in 2017-18, prime working-age adults who worked from home were more likely to prepare food (75 percent versus 63 percent) and to spend more time doing so (41 minutes compared with 30 minutes) than individuals who worked away from home. Individuals who worked from home spent 49 minutes eating at home, which was nearly double the amount reported by individuals who worked away from home (27 minutes). Teleworkers may consume a healthier diet if the greater time spent preparing food translates into eating more home-prepared meals and less eating out. Home-prepared meals tend to be lower in calories and higher in positive nutrients than meals prepared away from home, according to studies by ERS researchers. This chart appears in the ERS’ Amber Waves article, “Working From Home Leads to More Time Spent Preparing Food, Eating at Home,” February 2021.
Wednesday, August 12, 2020
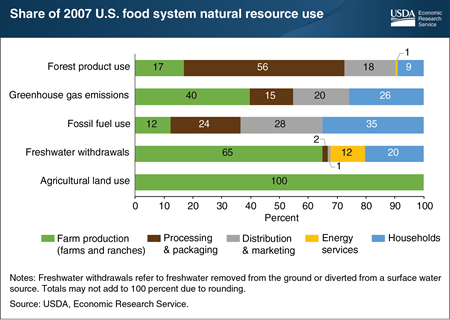
Knowing where natural resource use accumulates is fundamental to understanding what factors influence resource-use decisions. A recent Economic Research Service (ERS) study estimated natural resource use by the U.S. food system in 2007 (2007 data were the latest available with the level of detail needed for the analysis). Farm production was the smallest user of fossil fuels (12 percent of fossil fuel use); households were the largest users (35 percent). Over 40 percent of greenhouse gas emissions in food production were from farms and ranches, followed by households, and then companies that distribute and market food. For forest products, the greatest use occurred during food processing and packaging, with paper-based packaging accounting for most of this use. Farm production was the dominant user of freshwater withdrawals due to irrigation, but slightly over a third of water use by the food system in 2007 occurred after the farm, including in household kitchens (20 percent) and in the energy industry (12 percent). This chart appears in the ERS report, Resource Requirements of Food Demand in the United States, and Amber Waves article, “A Shift to Healthier Diets Likely To Affect Use of Natural Resources,” May 2020.
Thursday, May 28, 2020
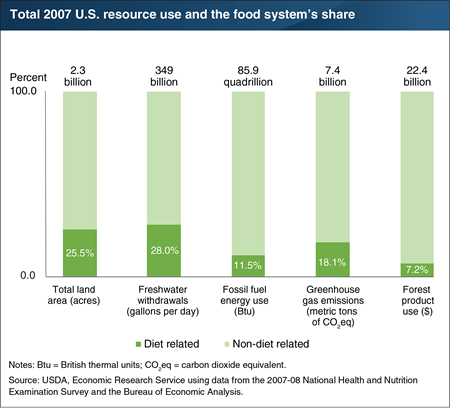
Conserving natural resources starts with identifying where they are used. A recent Economic Research Service (ERS) study examined how much of 5 of the Nation’s natural resources were used in 2007 to feed Americans aged 2 and above. (2007 data were the latest available with the level of detail needed for the analysis.) The researchers looked at the entire U.S. food system from production of farm inputs—such as fertilizers and feed—through points of consumer purchases in grocery stores and eating-out places to home kitchens. Their estimates show that agricultural land use in the U.S. food system was 25.5 percent of the country’s 2.3 billion acres of total land. Although the study does not account for other food-related land use, such as by forestry and mining industries serving the food system, it does show that about half of agricultural land is dedicated to food production for the U.S. market, and the other half was devoted to nonfood crops, like cotton and corn for producing ethanol, and to export crops, like soybeans. The U.S. food system also accounted for an estimated 28 percent of 2007’s freshwater withdrawals, 11.5 percent of the fossil fuel budget, and 7.2 percent of marketed forest products. Air is a natural resource that is degraded by the addition of greenhouses gases. The food system accounted for an estimated 18.1 percent of U.S. greenhouse gas emissions in 2007. A version of this chart appears in the ERS report, Resource Requirements of Food Demand in the United States, May 2020 and the Amber Waves feature article, “A Shift to Healthier Diets Likely To Affect Use of Natural Resources.”
Wednesday, April 15, 2020
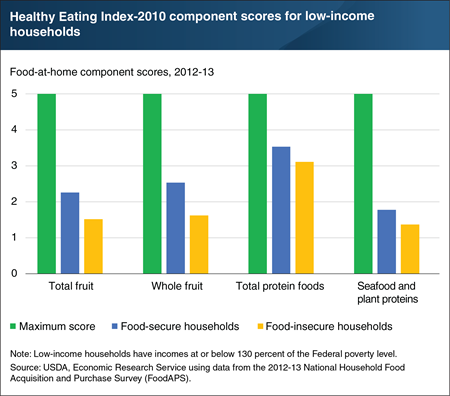
USDA monitors U.S. food security using a series of questions largely focused on whether a household can obtain sufficient quantities of food. However, the quality of foods acquired also affects personal wellbeing. USDA’s National Household Food Acquisition and Purchase Survey (FoodAPS) is unique among Federal surveys in that it collected information on both purchased foods and foods obtained for free, such as from food pantries and free school meals. Economic Research Service (ERS) researchers used FoodAPS data to examine the nutritional quality of a week’s worth of food at home—foods acquired at supermarkets, supercenters, farmers’ markets, convenience stores, and food pantries. The researchers focused on low-income households. They used the Healthy Eating Index-2010, which summarizes how well a set of foods compares to recommendations in the 2010 Dietary Guidelines for Americans, to assess diet quality. The index compiles scores for 12 components made up of specific food groups and subgroups. After controlling for individual- and household-level characteristics, only a handful of differences were associated with household food insecurity. For every 1,000 calories of food at home acquired, low-income food-insecure households acquired less total fruit, whole fruit, total protein, and seafood and plant proteins compared with low-income food-secure households. An extended version of this chart appears in “Food-Insecure Households Score Lower on Diet Quality Compared to Food-Secure Households,” in ERS’s March 2020 Amber Waves magazine.
Wednesday, March 18, 2020
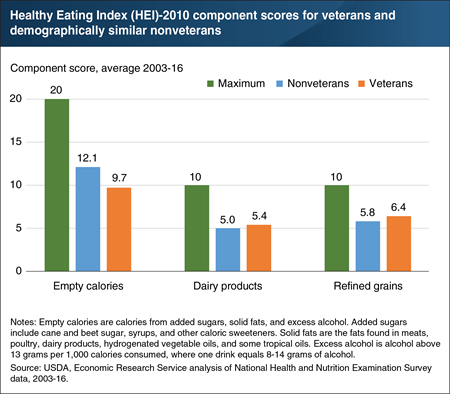
USDA and the National Cancer Institute developed the Healthy Eating Index (HEI) to measure how closely the foods and beverages that an individual consumes align with the Dietary Guidelines for Americans. Higher scores indicate a higher degree of compliance with recommendations. Economic Research Service (ERS) researchers used self-reported food intake data to compare veterans’ and nonveterans’ diets. After controlling for economic and demographic differences—for example, veterans tend to be older and are more often male—veterans’ and nonveterans’ average scores differed for three dietary components. Veterans scored higher on components for dairy products and refined grains, but lower on the empty calories component (meaning that empty calories accounted for a larger share of their total calories). In the HEI-2010, 12 component scores for specific food groups and subgroups—with maximum values ranging from 5 to 20—sum to a total score that measures overall diet quality, with a maximum value of 100. Veterans attained an average total HEI of 45.6 out of 100 versus 49.3 for nonveterans. The data for this chart come from the December 2019 ERS report, An Examination of Veterans’ Diet Quality. Veterans’ diet quality is also discussed in the February 2020 Amber Waves article, “Much Like Other Americans, Veterans Would Benefit From Improving the Quality of Their Diets.”
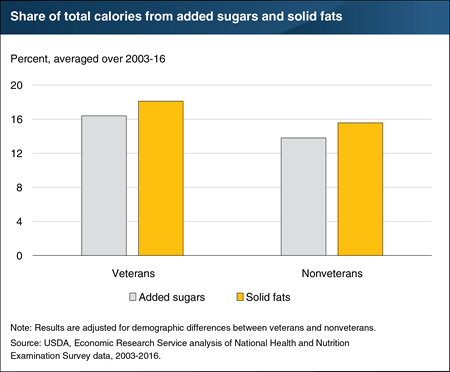
Wednesday, January 15, 2020
In a recent study, ERS researchers used self-reported food intake data to explore how veterans’ diets compare with those of nonveterans. The researchers found that, much like other Americans, veterans do not closely follow healthy eating recommendations in the Dietary Guidelines for Americans, jointly issued every 5 years by USDA and the Department of Health and Human Services. Veterans were found to have somewhat lower quality diets than nonveterans after controlling for demographic differences, such as the fact that veterans tend to be older and are more often male. Veterans’ lower diet quality was primarily due to their higher consumption of calories from added sugars and solid fats. Between 2003 and 2016, added sugars represented 16.4 percent of total calories for veterans, on average, versus 13.8 percent for demographically similar nonveterans. Added sugars include cane and beet sugar, syrups, and other caloric sweeteners. The Dietary Guidelines encourages individuals to keep calories from added sugars below 10 percent of total calories. Veterans obtained another 18.1 percent of their total calories from solid fats, as compared with 15.6 percent for nonveterans. Solid fats are the fats found in meats, poultry, dairy products, hydrogenated vegetable oils, and some tropical oils. The data for this chart come from the ERS report, An Examination of Veterans’ Diet Quality, December 2019.


