ERS Charts of Note
Subscribe to get highlights from our current and past research, Monday through Friday, or see our privacy policy.
Get the latest charts via email, or on our mobile app for  and
and 
Tuesday, April 9, 2024
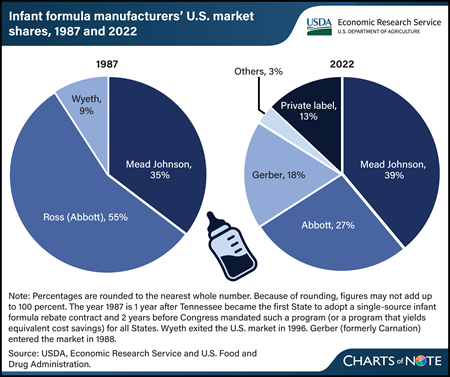
State agencies that administer USDA’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) use competitive, single-source contracts to reduce the cost of infant formula. These contracts provide significant discounts in the form of manufacturer rebates for each can of formula purchased through WIC. Infants who receive formula through WIC consume more than half of all infant formula in the United States. The manufacturer holding the WIC contract in a State sells the most infant formula in that State, including to consumers not participating in WIC. The infant formula market is highly concentrated. However, comparing market shares over time indicates that the market has become less concentrated. In 1987, the year of the first rebate contract and 2 years before Federal law required that WIC State agencies use cost containment systems, three manufacturers accounted for 99 percent of sales of infant formula in the United States. In 2022, three manufacturers accounted for 83 percent of sales of infant formula. In addition to WIC contracts with manufacturers, other factors influence infant formula market concentration, such as regulation of formula manufactured inside the United States and import restrictions on formula manufactured outside the United States. Entrances and exits of manufacturers and changes in their market shares over time suggest these factors impact firms differently. This chart appears in the USDA, Economic Research Service report The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): Background, Trends, and Economic Issues, 2024 Edition, published in February 2024.
Monday, April 8, 2024
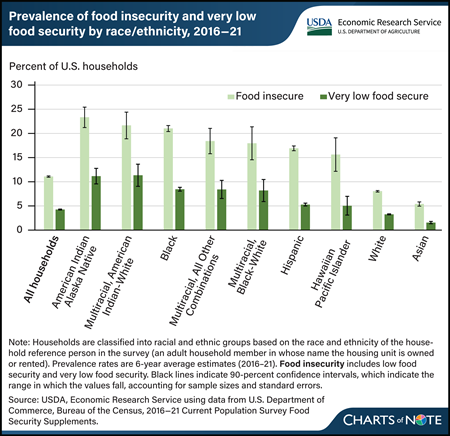
From 2016 to 2021, 11.1 percent of U.S. households experienced food insecurity, meaning they had difficulty providing enough food for all their members because of a lack of resources. Over the same period, 4.3 percent of U.S. households experienced very low food security, a more severe form of food insecurity in which food intake is reduced and eating patterns are disrupted. The prevalence of food insecurity during 2016–21 varied by race and ethnicity. Households headed by a reference person who identified as American Indian and Alaska Native (23.3 percent); Multiracial, American Indian-White (21.7 percent); Black (21.0 percent); Multiracial, All Other Combinations (18.4 percent); Multiracial, Black-White (18.0 percent); Hispanic (16.9 percent); and Hawaiian and Pacific Islander (15.6 percent) had significantly higher rates of food insecurity than the all-household average. The prevalence of food insecurity for households headed by a White (8.0 percent) or an Asian (5.4 percent) reference person was significantly lower than the all-household average. The prevalence of very low food security followed a similar pattern and was statistically significantly different from the all-household prevalence for most race and ethnicity categories. It was not significantly different for Hawaiian and Pacific Islander households. Very low food security ranged from 1.6 percent for Asian households to 11.3 percent for Multiracial, American Indian-White households. Meaningful differences in food insecurity exist across and within racial ethnic groups. Related data are available in the USDA, Economic Research Service report Household Food Insecurity Across Race and Ethnicity in the United States, 2016–21, published in April 2024.
Thursday, April 4, 2024
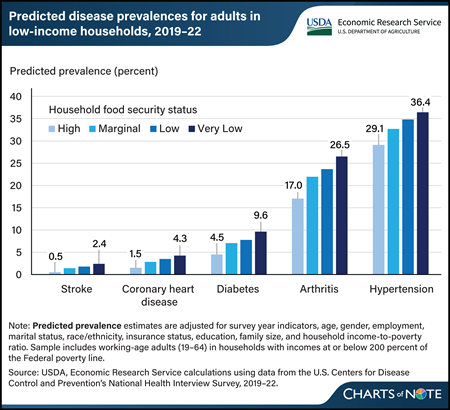
From 2019–22, the predicted prevalence of five selected chronic diseases was 1.9 to 9.5 percentage points higher for adults in very low food-secure households than those in high food-secure households. Researchers at USDA, Economic Research Service (ERS) recently updated estimates of the relationship between food security status and chronic disease among working-age adults in U.S. households with incomes at or below 200 percent of the Federal poverty level. They looked at the prevalence of stroke, coronary heart disease, diabetes, arthritis, and hypertension across four levels of household food security, ranging from high food security (households that reported no problems with or anxiety about being able to consistently obtain adequate amounts of food) to very low food security (in which eating patterns of one or more household members were disrupted and food intake was reduced). Adults in households that were less food secure were more likely to have one or more chronic disease, and the likelihood increased as food insecurity worsened. The prior data from 2011–15 and the more recent data from 2019–22 demonstrate a close link between food security status and health. This chart updates information in the ERS report Food Insecurity, Chronic Disease, and Health Among Working Age Adults, published in July 2017.
Monday, March 18, 2024
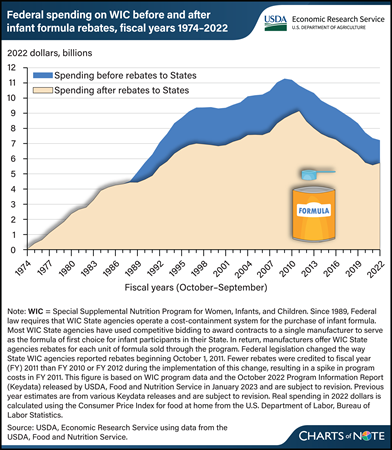
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serves to safeguard the health of low-income pregnant and postpartum women, infants, and children younger than 5 years who are at nutritional risk. State agencies responsible for implementing WIC use cost-containment strategies to reduce program costs. The greatest savings come from strategies used to contain the costs of providing infant formula through the program. Since 1989, most WIC State agencies have used competitive bidding to award contracts to a single manufacturer to serve as the formula of first choice for infant participants in their State. In return, manufacturers offer WIC State agencies rebates for each unit of formula sold through the program. From 1989 to 2022, savings to WIC from the rebates totaled $71.9 billion (in inflation-adjusted 2022 dollars), or 23 percent. Without the rebates, the Federal Government would have spent about $307.5 billion on the WIC program over that period. With the rebates, the Government spent $235.6 billion. This chart is drawn from the USDA, Economic Research Service report The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC): Background, Trends, and Economic Issues, 2024 Edition, published in February 2024.
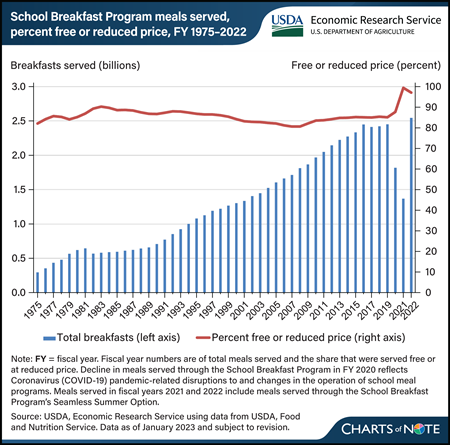
Monday, March 4, 2024
The USDA’s School Breakfast Program (SBP) has served about 63 billion meals since it was permanently authorized as a Child Nutrition Program in 1975. Any student in a participating school can get breakfast through the program. Students can receive a free breakfast if their household’s income is at or below 130 percent of the Federal poverty line (FPL), a reduced-price breakfast if their household’s income is between 130 and 185 percent of the FPL, and a full-price breakfast if their household’s income is above 185 percent of the FPL. The number of breakfasts served increased each year from 1982 through fiscal year (FY) 2016, before plateauing at about 2.4 billion meals from FY 2017 through FY 2019. On average, 85 percent of breakfasts were served for free or at a reduced price each year during this period. The onset of the Coronavirus (COVID-19) pandemic in March 2020 interrupted school operations, including the provision of meals, and the number of breakfasts served through the SBP dropped to about 1.8 billion breakfasts in FY 2020. The decrease reflected the use of USDA pandemic waivers, which allowed schools to serve meals through the Summer Food Service Program. From the end of FY 2021 through FY 2022, schools transitioned to serving meals through the SBP’s Seamless Summer Option. In FY 2022, the SBP provided 2.5 billion breakfasts, similar to prepandemic years. The data for this chart are from the USDA, Economic Research Service’s School Breakfast Program topic page.
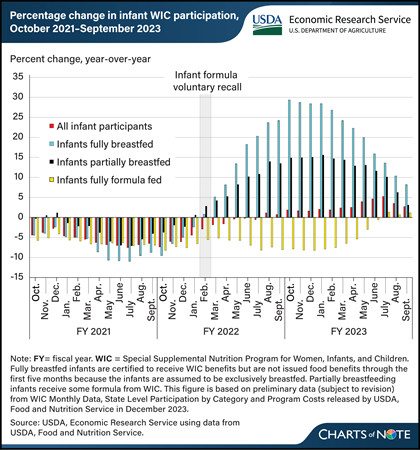
Tuesday, February 20, 2024
The number of breastfed infants in USDA’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) began to increase around the start of infant formula supply chain disruptions in 2022. In February 2022, a voluntary recall of some powder infant formulas and a temporary closure of a formula manufacturing facility compounded Coronavirus (COVID-19) pandemic-related supply chain issues that limited the supply of infant formula. National monthly WIC participation data provide insights into how caregivers of WIC-participating infants responded to these challenges. In March 2022, the number of fully formula feeding infants decreased 5 percent, while the number of partially breastfed infants increased 4 percent and the number of fully breastfed infants increased 5 percent compared with the same month in the previous year. By October 2022, the number of fully formula feeding infants had decreased 8 percent, while the number of partially breastfed infants increased 15 percent and the number of fully breastfed infants increased 29 percent from one year before. The increases in the numbers of breastfed infants continued in fiscal year 2023, remaining above previous year numbers through September. This chart is drawn from the USDA, Economic Research Service report The Special Supplemental Nutrition Program for Women, Infants, and Children: Background, Trends, and Economic Issues, 2024 Edition, published in February 2024.
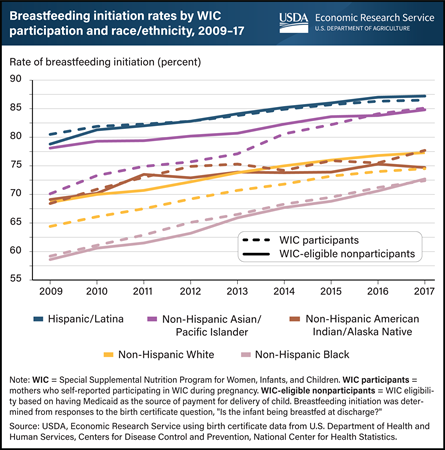
Tuesday, January 16, 2024
Breastfeeding is considered the best source of nutrition for infants and is therefore promoted by USDA’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Initiation, one breastfeeding metric, refers to breastfeeding an infant shortly after birth, including at or before discharge from the hospital. From 2009 to 2017, rates of breastfeeding initiation increased among low-income women regardless of WIC participation status or race/ethnicity. Hispanic women had the highest rates of breastfeeding initiation throughout the study period. Non-Hispanic Black women had the lowest rates of breastfeeding initiation, but they experienced the largest gains (22.3 percent among WIC participants and 24.1 percent among WIC-eligible nonparticipants). Compared with WIC-eligible nonparticipants (80.1 percent), WIC participants (78.5 percent) continued to have lower rates of breastfeeding initiation overall, although the gap in initiation between WIC-eligible nonparticipants and WIC participants closed for some racial/ethnic groups. In 2009, Asian/Pacific Islander women had the largest gap in breastfeeding initiation by WIC status. By 2017, this gap had narrowed and reversed direction because of a greater increase in breastfeeding initiation among WIC participants (21.4 percent) compared with WIC-eligible nonparticipants (8.6 percent). This pattern also was observed for American Indian/Alaska Native women and for non-Hispanic White women. This chart appears in the USDA, Economic Research Service’s Amber Waves article Rates of Breastfeeding Initiation Increased Among Low-Income Women, 2009–17; Racial and Ethnic Disparities Persist, released October 2023.
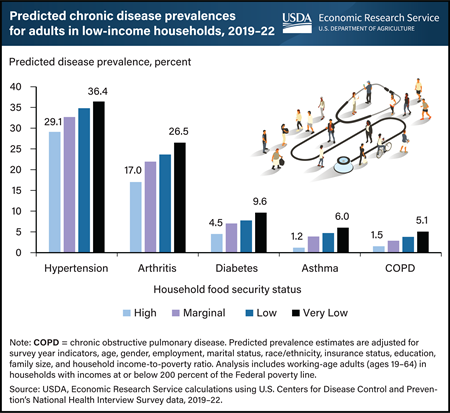
Monday, January 8, 2024
Adults in U.S. households that are less food secure are significantly more likely to have one or more chronic diseases, and the likelihood increases as food insecurity worsens. Researchers at USDA, Economic Research Service (ERS) recently updated estimates of the fraction of working-age adults with chronic disease in households with incomes at or below 200 percent of the Federal poverty level based on food security status using data from 2019–22. They looked at the rate of five chronic diseases across four levels of household food security, ranging from high food security (households with no problems or anxiety about consistently obtaining adequate food) to very low food security (eating patterns of one or more household members were disrupted and food intake reduced). From 2019–22, predicted illness prevalences among the five chronic diseases examined were 3.6 to 9.5 percentage points higher for adults in very low food-secure households compared with those in high food-secure households. This shows that food security status and health are closely linked. This chart updates information in the Amber Waves article, Adults in Households With More Severe Food Insecurity Are More Likely To Have a Chronic Disease, published in October 2017, and in the ERS report Food Insecurity, Chronic Disease, and Health Among Working-Age Adults, published in July 2017.
Wednesday, January 3, 2024
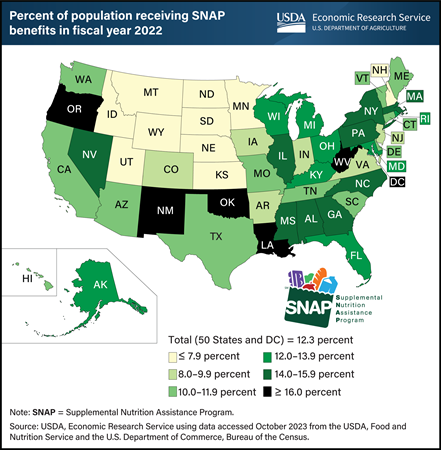
In fiscal year (FY) 2022, USDA’s Supplemental Nutrition Assistance Program (SNAP) served an average of 41.1 million people per month in the 50 States and Washington, DC. SNAP is the largest domestic nutrition assistance program, accounting for about two-thirds of USDA spending on food and nutrition assistance in recent years. The SNAP participation rate increased nationwide during the Coronavirus (COVID-19) pandemic, to a high of 12.5 percent of the resident population of the 50 States and DC in FY 2021. The FY 2022 rate fell slightly to 12.3 percent. SNAP participation varies across States because of differences in program administration and economic conditions. In FY 2022, the share of residents receiving SNAP benefits in each State ranged from as high as 24.5 percent in New Mexico to as low as 4.6 percent in Utah. In 35 States, the share was somewhere between 8 and 16 percent. This map appears in USDA, Economic Research Service’s Charting the Essentials, last updated November 2023.
Tuesday, December 12, 2023
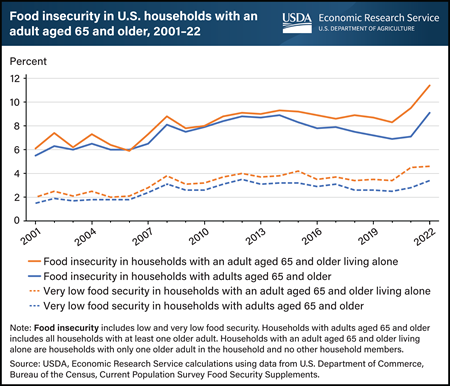
In 2022, 9.1 percent of U.S. households with adults aged 65 and older were food insecure at some time during the year, meaning they had difficulty providing enough food for all their members because of a lack of resources. The prevalence of food insecurity in households with adults aged 65 and older in 2022 was statistically significantly higher than the 7.1 percent in 2021 and the 6.9 percent in 2020. USDA, Economic Research Service monitors the food security status of households in the United States through an annual nationwide survey. The survey does not include older adults residing in assisted living facilities. In 2022, 11.4 percent of households with an adult aged 65 and older living alone were food insecure, which is statistically significantly higher than the prevalence in 2021 of 9.5 percent and in 2020 of 8.3 percent. Very low food security is a more severe form of food insecurity in which the food intake of some household members was reduced and normal eating patterns were disrupted at times during the year. The 2022 prevalence of very low food security in households with adults aged 65 and older was 3.4 percent, statistically significantly higher than the 2.8 percent in 2021 and the 2.5 percent in 2020. Household food security data by various demographic categories, such as older adults, are available in the report Household Food Security in the United States in 2022, published in October 2023.
Thursday, December 7, 2023
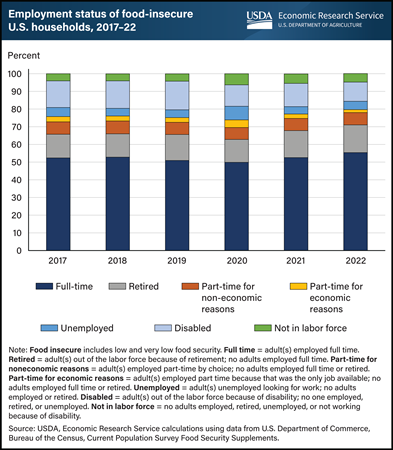
In 2022, over half of all food-insecure households in the United States had one or more adult members employed full time. USDA, Economic Research Service (ERS) monitors the prevalence of U.S. household food insecurity through an annual survey and provides information about the characteristics of food-insecure households, including their employment status. The employment status for each household is measured using the combined employment status of all adult household members. In 2022, households with adults employed full-time made up the largest share of food-insecure households at 55 percent, a share that has remained stable since 2017. Households with one or more adults employed part time because it was the only job available (called part time for economic reasons) comprised the smallest share of food-insecure households at 2 percent. The remaining food-insecure households had one or more adults who were retired, employed part time for non-economic reasons, unemployed, disabled, or not in the labor force. An interactive visualization and the underlying downloadable data for prevalence, severity (low and very low food security), and distribution of food insecurity by household employment status can be found on the ERS Interactive Charts and Highlights page.
Monday, October 30, 2023
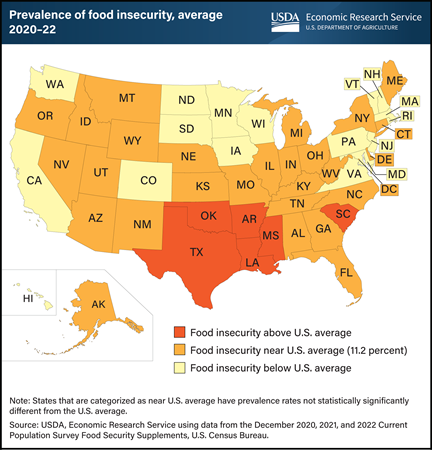
Food-insecure households sometimes have difficulty providing enough food for all their members because they lack resources. USDA, Economic Research Service (ERS) monitors the extent of food insecurity in U.S. households at the national and State levels through an annual U.S. Census Bureau survey. State-level estimates are obtained by averaging 3 years of data to generate a larger sample size in each State. This provides more precise estimates and more power to detect differences across States. The estimated prevalence rates of food insecurity during 2020–22 ranged from 6.2 percent in New Hampshire to 16.6 percent in Arkansas. The estimated national 3-year average for all States was 11.2 percent. The prevalence of food insecurity was statistically significantly higher than the national average in 6 States (AR, LA, MS, OK, SC, and TX) and statistically significantly lower than the national average in 17 States (CA, CO, HI, IA, MA, MD, MN, ND, NH, NJ, PA, RI, SD, VA, VT, WA, and WI). In the remaining 27 States and the District of Columbia, differences from the national average were not statistically significant. An interactive food insecurity map can be found on ERS’s Interactive Charts and Highlights page that allows users to view two measures of food insecurity over multiple years for each State. Users can see State trends in food insecurity, how States compare with national food insecurity prevalence rates, and how States compare with one another. This map appears on ERS’s Key Statistics & Graphics page.
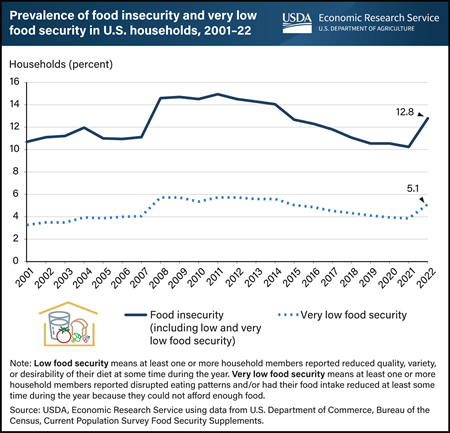
Wednesday, October 25, 2023
In 2022, 12.8 percent of U.S. households (17 million) were food insecure at some time during the year, meaning they had difficulty providing enough food for all their members because of a lack of resources. The prevalence of food insecurity in 2022 was statistically significantly higher than the 10.2 percent recorded in 2021 and the 10.5 percent in 2020. USDA, Economic Research Service (ERS) monitors the food security status of households in the United States through an annual nationwide survey. Very low food security is a more severe form of food insecurity in which the food intake of some household members was reduced and normal eating patterns were disrupted. The 2022 prevalence of very low food security was 5.1 percent, statistically significantly higher than the 3.8 percent in 2021 and the 3.9 percent in 2020. This chart appears on ERS’s Key Statistics & Graphics page and in the ERS report Household Food Security in the United States in 2022, published October 25, 2023.
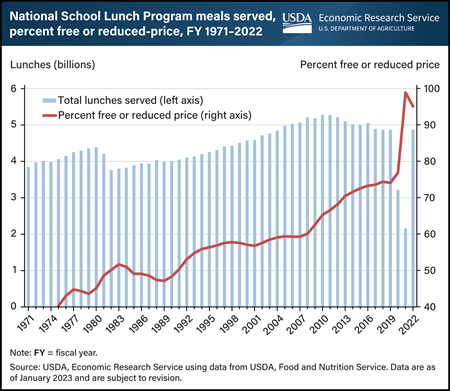
Tuesday, October 10, 2023
The USDA’s National School Lunch Program (NSLP) served 4.9 billion lunches in fiscal year 2022, and about 228.9 billion lunches since 1971. Any student in a participating school can get an NSLP lunch. Typically, students may be eligible for either a free, reduced-price, or full-price lunch depending on their household’s income. Compared with previous years, a higher share of the lunches were served for free or at a reduced price in fiscal years 2020 through 2022. This was in large part because of USDA waivers during the Coronavirus (COVID-19) pandemic allowing for meals to be provided free of charge to all students. These waivers expired in June 2022. The onset of the pandemic in March 2020 interrupted the operations of many schools, disrupting the provision of lunches through the NSLP. In response, USDA allowed schools to serve free meals through the Summer Food Service Program or the NSLP’s Seamless Summer Option, while the temporary Pandemic Electronic Benefit Transfer program reimbursed eligible families for the value of school meals missed because of these disruptions. This chart appears on the USDA, Economic Research Service’s National School Lunch Program page within the Child Nutrition Programs topic page.
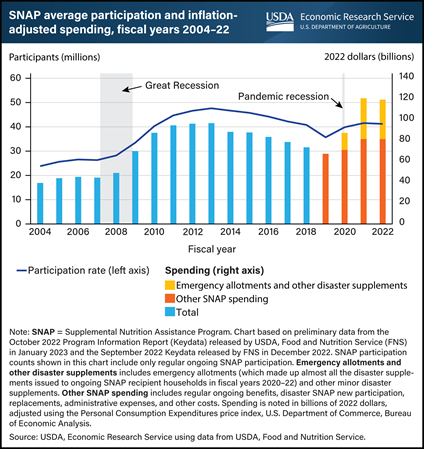
Wednesday, August 23, 2023
USDA’s Supplemental Nutrition Assistance Program (SNAP) is designed to expand during economic downturns. SNAP participation and inflation-adjusted spending grew each year from fiscal year (FY) 2007–13 following the Great Recession and from FY 2019–21 following the recession caused by the Coronavirus (COVID-19) pandemic. However, aspects of program growth differed between these periods. Average monthly participation increased faster, for longer, and by a greater amount following the Great Recession than it did after the COVID-19 recession, peaking at 47.6 million participants in FY 2013. Although participation grew less from FY 2019–21, inflation-adjusted spending rose more quickly given the shorter time span, from $67.5 billion in FY 2019 to $120.8 billion in FY 2021 (an average 39.5-percent increase per year). Emergency allotments were central to SNAP spending growth during the pandemic. Emergency allotments were issued as monthly supplements in response to the pandemic, bringing all recipients’ benefits to the maximum allowed each month beginning in 2020 (and later providing a minimum of $95 per month for all recipients). In FY 2021, emergency allotments and other disaster supplements accounted for $39.2 billion, almost a third of total spending. Excluding spending on emergency allotments and other disaster supplements, total spending was only $81.6 billion in FY 2021, about $15 billion less than FY 2013 spending, adjusting for inflation. Emergency allotments ended in 17 States over FY 2021–22 and in the remainder of States in early 2023. This chart appears in the USDA, Economic Research Service’s Amber Waves article, U.S. Food and Nutrition Assistance Programs Continued To Respond to Economic and Public Health Conditions in Fiscal Year 2022, released August 2023.
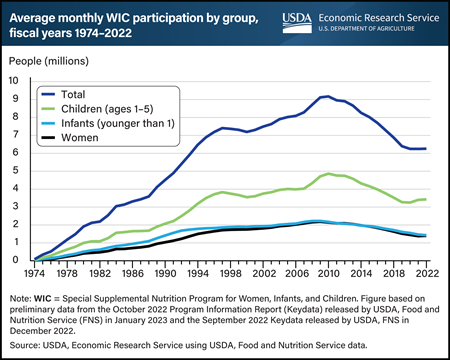
Tuesday, August 8, 2023
USDA’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides supplemental food packages, nutrition education, breastfeeding support, and health care referrals at no cost to low-income pregnant and postpartum women, infants younger than 1 year old, and children 1 to 5 years old who are at nutritional risk. More than half of WIC participants are children (54.8 percent), followed by infants (22.8 percent) and women (22.4 percent). Total participation in WIC increased for the first time in more than a decade in fiscal year (FY) 2022. Participation averaged 6.26 million people a month, up from 6.24 million a month in FY 2021. This was the first increase in overall participation since the record high 9.18 million in FY 2010 and resulted from increased numbers of women and children participants. Women participants increased by 1.5 percent in FY 2022 after declining for the previous 12 fiscal years, whereas infant participants continued to decline. Declines in the number of births in the United States, beginning in 2008, may be a factor in drops in infant participation. Child participation increased in FY 2022 for the second consecutive fiscal year. Administrative flexibilities put in place in response to the Coronavirus (COVID-19) pandemic may have helped support participation, especially among children. Starting in FY 2020 and continuing through FY 2022, USDA waivers temporarily allowed State agencies to conduct remote certifications for applicants and recertifications for WIC participants and to extend certification periods for certain WIC participants by up to 3 months. This chart appears in the USDA, Economic Research Service’s Food and Nutrition Assistance Landscape: Fiscal Year 2022 Annual Report, released June 21, 2023.
Tuesday, August 1, 2023
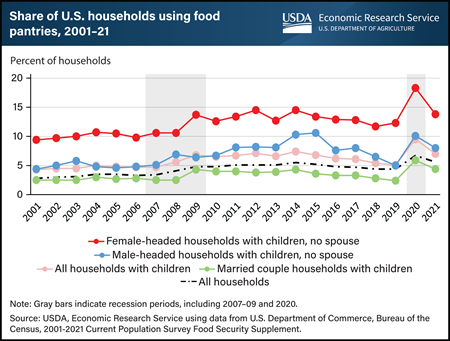
During the past 20 years, households with children headed by a single female consistently showed higher average rates of food pantry use than other household types, including male-headed households with children and married couple households with children. The cost of childcare, education, healthcare, housing, and other expenses can strain a family’s budget, leaving less income available for food purchases. This financial strain may lead parents to seek assistance from food pantries to meet their families’ food needs. Food pantries, often affiliated with faith-based organizations, typically provide free food for people to take home and prepare. The use of food pantries increased in 2009 during the end of the Great Recession and increased in 2020 during the Coronavirus (COVID-19) pandemic, with average rates increasing more than any previous year. In 2021, 7 percent of households with children used food pantries at some point during the year, compared with 5.6 percent of all households. Among households with children, 4.4 percent of married-couple households used food pantries, while 13.8 percent of single female-headed households and 8 percent of single male-headed households used them. Food pantry use among households with children headed by females fluctuated from 9.4 percent in 2001 to 18.3 percent in 2020. The data for this chart come from the USDA, Economic Research Service’s 2001-2021 annual reports on Household Food Security in the United States. The release of the 2022 Household Food Security in the United States report and corresponding statistical supplement is scheduled for October 25, 2023, because of updates to the survey instrument implemented in 2022.
Wednesday, June 21, 2023
USDA, Economic Research Service (ERS) released “The Food and Nutrition Assistance Landscape: Fiscal Year 2022 Annual Report” on Wednesday, June 21, 2023. The report examines program trends and policy changes in USDA’s largest domestic food and nutrition assistance programs through fiscal year 2022. An overview of the annual ERS report will be provided in a webinar at 1 p.m. EDT, Wednesday, June 21. To join or register, click here.
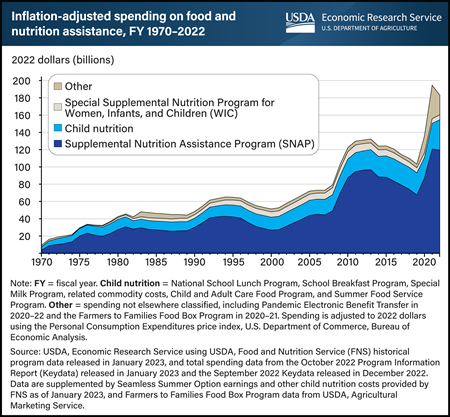
Federal spending on USDA’s food and nutrition assistance programs totaled $183.0 billion in fiscal year (FY) 2022, down 6 percent from the record-high spending of $194.7 billion in FY 2021, adjusted for inflation to 2022 dollars. Before adjusting for inflation, total FY 2021 spending was $183.3 billion. In FY 2022, the Supplemental Nutrition Assistance Program (SNAP) maximum allotment permanently increased after the Thrifty Food Plan was re-evaluated, and several States also ended SNAP emergency allotments, which temporarily raised all recipients’ benefits to at least the maximum for their household size. SNAP spending totaled $119.5 billion in FY 2022, 1 percent less than the inflation-adjusted record-high spending in FY 2021. Spending on the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) totaled $5.7 billion—an increase of 7 percent from inflation-adjusted spending in FY 2021—reflecting an increase in program food costs per participant. Combined spending on child nutrition programs totaled $35.1 billion in FY 2022, increasing 19 percent from the inflation-adjusted total in the previous year. This increase was driven by a greater number of meals served through these programs in FY 2022 compared with FY 2021, as well as higher reimbursement rates for meals served. Combined spending on other programs fell in FY 2022 primarily because of lower spending on Pandemic Electronic Benefit Transfer (P-EBT) and the expiration of the Farmers to Families Food Box Program midway through FY 2021. This chart is based on data available as of January 2023 and appears in the USDA, Economic Research Service’s Food and Nutrition Assistance Landscape: Fiscal Year 2022 Annual Report, released June 2023.
Thursday, April 6, 2023
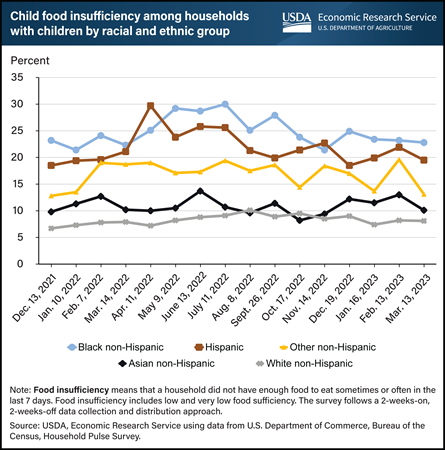
In March 2023, 22.8 percent of Black non-Hispanic households reported that their children sometimes or often did not have enough to eat during the past week. Additionally, 19.5 percent of Hispanic households, 13.1 percent of Other non-Hispanic, 10.1 percent of Asian non-Hispanic, and 8.1 percent of White non-Hispanic households reported child food insufficiency. The Household Pulse Survey, which provides these food insufficiency estimates, was developed through a partnership with the U.S. Census Bureau to produce timely information on the economic and social effects of the Coronavirus (COVID-19) pandemic on U.S. households. Households were classified as having child food insufficiency if the adult survey respondent said children in the household were not eating enough “sometimes” or “often” in the last 7 days because the household could not afford enough food. The prevalence of child food insufficiency for Hispanic households with children peaked in April 2022 at 29.7 percent, while Black non-Hispanic households with children experienced similarly high rates in May (29.2 percent), June (28.7 percent), and July (30.0 percent) of 2022. In contrast, White non-Hispanic households with children experienced a high of just more than 10 percent in August 2022, and Asian households with children reached a high of 13.7 percent in June 2022. The prevalence of child food insufficiency for Other non-Hispanic households with children has fluctuated between these two groups during the same time period. While the prevalence of child food insufficiency for some groups declined from peak levels by March 2023, it continues to affect certain groups more than others. For more information on the USDA, Economic Research Service’s food security research and comparisons of food insecurity and food insufficiency measurements, see the Food Security in the U.S. topic page on the website. This chart appears on the Food Sufficiency During the Pandemic trending topics page.
Monday, November 14, 2022
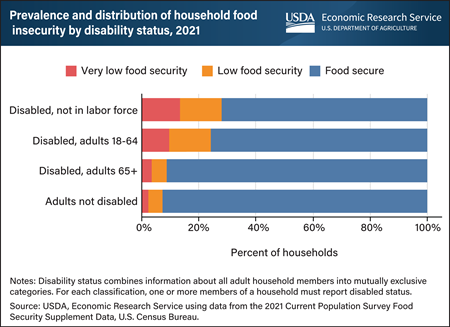
In 2021, households that included an adult with disabilities reported higher food insecurity rates than households with no adults with disabilities. Food-insecure households are those that had difficulty at some time during the year providing enough food for all their members because of a lack of resources. In 2021, for U.S. households that included an adult out of the labor force because of a disability, 28 percent were food insecure (low and very low food security). Among U.S. households with an adult age 18-64 who reported a disability but was not out of the labor force because of it, 24 percent were food insecure. In contrast, 7 percent of households with adults without disabilities were food insecure in 2021. Households that include at least one adult 65 and over who reported a disability had food insecurity prevalence rates similar to households with adults without disabilities (9 percent). Very low food security, the more severe form of food insecurity in which normal eating patterns were disrupted and the food intake of some household members was reduced, was also higher for households that included adults with disabilities. In 2021, the prevalence rate of very low food security for households that included adults not in the labor force because of a disability was more than five times that of households that included adults without disabilities (13 percent compared with 2 percent of households). Households that include adults ages 18–64 with a disability, but not out of the labor force because of the disability, also experienced higher prevalence rates of very low food insecurity at 10 percent. This chart appears in USDA, Economic Research Service’s Interactive Charts and Highlights page.


